
Exploring environmental design attributes impacting staff perceptions of safety in a complex hospital system: implications for healthcare design
Highlight box
Key findings
• The study found certain factors significantly influenced staff satisfaction with safety. These included patient privacy, space adjacency, positive distractions, clear signage, cleanliness, and flooring quality, which predicted staff satisfaction with patient and visitor safety. Additionally, security, staff privacy, team visibility, and comfortable furniture were significant predictors of staff satisfaction with perceptions of safety.
What is known and what is new?
• This study reaffirms the existing knowledge regarding the influence of environmental design on satisfaction with patient and staff safety. Furthermore, it contributes novel insights by pinpointing latent elements, including positive distraction, spatial layout, signage, and comfortable furniture, as significant predictors of staff satisfaction regarding safety perceptions.
What is the implication, and what should change now?
• By addressing the identified factors collectively, they contribute to creating healthcare spaces that adhere to regulatory standards and prioritize the safety, satisfaction, and effectiveness of staff and patients, ultimately improving the quality of care and minimizing adverse incidents in healthcare settings.
Introduction
Background
Healthcare safety is a global priority recognized by the World Health Organization (WHO). It encompasses the safety of patients and staff, which is vital for delivering quality care and measuring hospital performance (1). Patient safety, which refers to preventing harm in healthcare settings, according to the Agency for Healthcare Research and Quality (AHRQ), is closely connected to staff safety (2). The design of healthcare facilities plays a significant role in ensuring safety. Research has highlighted its influence on mitigating various factors such as stress, aggression, violence, medical errors, security, visibility, privacy, staff communication, infection transmission, and falls (3-11). However, there is a pressing need for further research to delve deeper into staff perceptions of safety and how the physical environment can be strategically optimized to enhance safety comprehensively.
The following sections explore the relationship between the physical environment and safety in healthcare settings, examining patient and staff privacy, efficient spatial planning, positive distractions, cleanliness, fall prevention, security measures, team visibility, and furniture ergonomics. Understanding how these elements influence safety is crucial for creating healthcare settings that prioritize the well-being of all individuals involved. Continuous research, evaluation, and improvement are essential to staying abreast of evolving best practices and adapting to emerging challenges, ultimately creating settings that support the highest standards of healthcare safety and the well-being of all those within the healthcare environment.
Patient and staff privacy
Designing for patient privacy is essential for safety and patient satisfaction (8,12-15). Healthcare institutions are legally obligated to uphold patient privacy through the Health Information Portability and Accountability Act (HIPAA), which prevents unauthorized information sharing (16). This is particularly crucial for medical conditions that carry stigmas, as it prevents community harm and social shame (12). Furthermore, creating acoustically private environments within healthcare settings fosters patient trust (8,17). This trust is critical in ensuring secure communication of medical information and enhancing the perceived quality of care (8). In summary, prioritizing patient privacy in healthcare design adheres to legal mandates and contributes to a healthcare environment where patients can trust in the confidentiality of their information and the quality of care they receive.
Staff privacy in healthcare extends beyond individual rights; it significantly influences staff perceptions of safety and patient outcomes (13,14,17-21). It establishes a psychologically safe workplace where employees feel comfortable voicing concerns, fostering an atmosphere of accountability and improving patient safety (8,21). Moreover, staff privacy cultivates trust among healthcare teams, facilitating effective communication, reducing errors, and leading to enhanced safety outcomes (19,21-24). For instance, Naccarella (24) found that Emergency Department (ED) staff navigate the balance between visual openness and connectedness to the wider ED and the need for privacy and confidentiality by strategically using different spaces for various types of communication. The visual transparency of EDs posed challenges for staff engaging in confidential, informal communication, as they were concerned about being overheard by others in open areas, feeling vulnerable to peer, patient, and family scrutiny, and navigating informal communication norms and perceptions of work events. In conclusion, prioritizing staff privacy in healthcare settings is fundamental to creating a safe and efficient care environment that benefits both healthcare providers and patients.
Space planning
Effective spatial planning within healthcare facilities has a substantial impact on the safety of both staff and patients, as evidenced by research findings (6,9,25,26). Notably, the distances clinicians’ traverse is a known factor contributing to staff fatigue, heightened stress levels, and susceptibility to interruptions, all of which can compromise patient safety (27-29). For instance, Chaudhury et al. (9) found that extended walking distances for healthcare staff increased stress and diminished care efficiency.
Various design interventions have been proposed to address these challenges and improve wayfinding. These include the implementation of effective signage, informative printed materials, prominent landmarks, thoughtfully chosen color schemes, enhanced visibility, appropriate furniture, and interior elements, and the integration of navigational technologies (13,30,31). Inadequate wayfinding can lead to many issues in healthcare settings, including stress, patient absenteeism, tardiness, aggression, or frustration (13,30,31). For example, Zamani (13) highlighted safety concerns arising from wayfinding difficulties in an ED, underscoring the importance of clear signage and enhanced visibility. Despite recognizing the significance of efficient wayfinding, limited research directly establishes a link between wayfinding challenges and safety outcomes (31). Further investigation is imperative to understand how spatial planning can influence safety, thereby enhancing the well-being of patients and staff within healthcare facilities.
Cleanliness
Maintaining cleanliness in healthcare spaces is of utmost importance for infection control (7,32,33). Contamination can spread through direct contact with patients, surfaces, or healthcare workers’ hands (10,34-37). For instance, Durant (37) reported that patients who reported their rooms as “always” clean had significantly lower rates of HA difficile Infection (HA-CDI). However, it’s crucial to recognize that existing guidelines for cleaning and disinfection in healthcare facilities may fall short (10,34-36,38). In another study, Carling and colleagues (38) marked high-touch surfaces with ultraviolet (UV)-visible substances and found only 47% adequacy in cleaning out of 1,404 marked surfaces in three hospitals. Additional strategies include automated disinfection systems such as hydrogen peroxide vapors, UV light, pulsed xenon UV light, and self-disinfecting surfaces (35). In summary, ensuring cleanliness is vital for infection prevention, ultimately enhancing patient safety and reducing the risk of healthcare-associated infections.
Falls
Falls represent the most prevalent safety incidents in healthcare settings, particularly among older patients (11,39-42). Various studies have identified environmental factors contributing to the increased risk of falls in patient rooms, such as inadequate lighting, increased turning angles to reach destinations, slippery floors, space configurations affecting posture, tightness of space, and limited visitor space (11,29,40-44). For example, Pati et al. (41) highlighted a strong association between smaller turns, up to 90 degrees, and fall initiation, with only a complete 180-degree turn angle showing statistical significance. On a broader scale, studies have demonstrated that unobstructed and efficient access for caregivers from corridors to patient beds, improved patient head visibility, and unit design enhancing visibility are linked to reduced fall rates (29,40,44). Further research is needed to understand the perceived impact of extrinsic environmental factors in healthcare settings on fall incidents, guiding the development of fall prevention strategies to improve safety perceptions.
Security
Security in healthcare, an essential component of safety, exhibits complex connections with operational efficiency due to the potential disruption caused by aggressive incidents (5,45-47). These security events affecting staff stem from extended waiting times, delays, aggression, patient stress, visitor issues, and substance abuse (5,45,48). To enhance security, recommendations include strategically positioning security personnel and clinical staff for improved visibility and team proximity, enhancing visual access to entrances and exits, and establishing dedicated areas for aggressive patients (13,23,49,50).
This is highlighted by Pati and colleagues (45) study, that pinpointed the walk-in entry in the ED as the most vulnerable security point for both staff and patients. Such findings underscore the importance of unobstructed visibility from registration, triage, and security desk areas to maintain ED operations and safety. Furthermore, Zamani (13) suggested creating a separate and tranquil waiting space with ample visibility for behavioral health (BH) patients to enhance security in ED settings. Additionally, participants in the study recognized the significance of having an adequate number of security guards in areas with a direct line of sight to entrance doors, along with the necessary training to handle “code gray” situations involving aggressive behaviors, which was perceived as crucial. In summary, prioritizing security safeguards individuals and property and contributes to a safer and more efficient care delivery system in healthcare environments.
Team visibility
Effective healthcare facility design enhances team visibility among staff members, fostering a sense of proximity, connectedness, and improved communication (13,23,24). This aspect of design plays a pivotal role in shaping the dynamics of teamwork among healthcare professionals, including physicians, nurses, and support staff, ultimately influencing efficiency and safety outcomes (5,24,49,51,52).
When healthcare facility design prioritizes team visibility, staff members are readily available to support one another in addressing security or safety concerns, creating an environment that promotes collective well-being (24,49). For instance, a study conducted by Naccarella (24) underscores the consistent emphasis placed by staff on the importance of both auditory and visual awareness within the healthcare setting, particularly in the ED. This heightened awareness not only enables staff to monitor ongoing events effectively but also helps them maintain situational awareness. Such awareness is paramount in enhancing staff and patient safety, including the early detection and effective management of potential hazards such as violence or aggression.
Various design elements contribute to enhancing peer visibility, including the implementation of open layouts, wider corridors, nurse stations positioned at counter height, strategically located nurse stations, and the integration of transparency between team stations or team rooms (13,23,24,49,53). By incorporating these visibility-enhancing design elements, healthcare facilities are prone to creating a safer and more collaborative environment for their staff, ultimately improving the quality of care and patient outcomes.
Furniture and equipment ergonomics
Existing evidence underscores the compelling need to integrate ergonomic considerations into healthcare facility design, particularly concerning the size, form, angles, and clearances of workstations, chairs, desks, and various equipment, all of which should be customizable and adjustable to cater to individual user needs (54-56). Ergonomically designed furniture and equipment play a pivotal role in enhancing the overall performance of healthcare workers while simultaneously mitigating the risk of work-related musculoskeletal disorders (WMSD) (25,55-60). These ergonomic considerations acknowledge the unique needs and preferences of healthcare professionals and align with the broader goal of creating a workspace that prioritizes both comfort and efficiency, ultimately contributing to the well-being of staff and the quality of care they provide.
In summary, understanding the impact of the physical environment on patient and staff safety is crucial for creating healthcare settings that prioritize the well-being of all individuals involved. Continuous research, evaluation, and improvement are essential to staying abreast of evolving best practices and adapting to emerging challenges, ultimately creating settings that support the highest standards of healthcare safety and the well-being of all those within the healthcare environment.
Positive distraction
Due to illness-related factors, healthcare environments often induce stress and anxiety in patients and staff (61,62). The relationship between positive distractions in healthcare settings and patient safety outcomes has been a topic of interest among researchers (63-65). Positive distractions refer to stimuli intentionally designed to enhance the sensory experiences of patients, produce positive feelings, and hold attention without burdening or stressing the individual, blocking worrisome thoughts (62,66).
Designing healthcare facilities with features like calming music, pleasing colors, engaging stimuli, natural light, and scenic views introduces positive distractions that enhance patient and staff safety (4,62-65,67). For example, a study by Beukeboom et al. (64) revealed that the presence of natural plants and posters reduced patients’ stress levels. Vetter et al.’s (65) comprehensive literature review further emphasized the positive impact of art forms, music, natural imagery, spacious rooms, and sunlight in mitigating patient anxiety and pain. Moreover, Kim et al. (63) demonstrated the effectiveness of allowing patients to choose music during surgery, showing a reduction in intraoperative anxiety and improved safety outcomes. These findings emphasize the potential of positive distractions to mitigate stress and anxiety, enhancing safety for patients and staff. Incorporating such elements into healthcare facility design and management is a valuable strategy for promoting overall well-being and safety.
Rationale and knowledge gap
This study is driven by the critical necessity to prioritize safety within healthcare environments, safeguarding the interests of both patients and staff. Incidents compromising safety in healthcare settings carry significant repercussions, including potential patient harm, heightened healthcare expenditures, and declining staff morale. Consequently, a comprehensive understanding of the factors contributing to safety outcomes becomes imperative for healthcare organizations to develop and implement effective risk mitigation strategies and ultimately enhance overall safety.
The Job Demands-Control-Support (JDCS) model is a valuable framework aligned with the rationale for this study (68,69). Recognized for its ability to elucidate how job-related factors impact employees’ psychological well-being, the JDCS model encompasses critical dimensions such as job demands, control over work, and social support in the workplace (69). This model proves particularly pertinent when examining the influence of environmental factors on staff safety perceptions, as it delves into the intricate interplay between job demands, control, and support in shaping employees’ overall well-being (68). In the context of this study, the JDCS model furnishes a solid theoretical foundation for exploring the specific environmental factors that contribute to staff satisfaction with safety perceptions. By contextualizing these elements within the framework of the JDCS model, researchers can effectively unravel their role in shaping the psychological well-being of healthcare staff and their overall safety perceptions.
Purpose
The primary aim of this study was to assess how various physical environment attributes impact staff satisfaction with safety, encompassing staff, patients, and visitors, and to elucidate the integration of these findings into our facility planning and design approach. This research is rooted in the global recognition of healthcare safety as a top priority, acknowledged by influential organizations such as WHO and the JDCS model. Safety in healthcare settings is of utmost significance, encompassing the well-being of both patients and staff. Adequate safety measures contribute to the quality of care and serve as crucial performance indicators for healthcare facilities.
However, existing research has revealed substantial gaps, particularly in understanding how the physical environment influences safety perceptions among clinical and non-clinical staff in healthcare settings. To address these critical gaps, this study is meticulously designed to thoroughly investigate the satisfaction levels associated with specific attributes of the physical environment. Through this research, we aim to uncover valuable insights into the factors that significantly impact staff satisfaction with safety, whether related to patients or visitors.
This research endeavor aspires to make a substantial contribution to the field of healthcare safety by providing a nuanced understanding of how various physical environment attributes influence safety perceptions among staff. These insights will enrich the existing body of knowledge and offer practical guidance to healthcare organizations as they strive to enhance safety measures and create more secure and supportive environments for their personnel and those they serve. Ultimately, this study seeks to bridge critical research gaps and facilitate evidence-based decision-making to comprehensively improve safety in healthcare settings.
Methods
The Healthcare System being examined is a prominent healthcare network in Central New York. It encompasses a vast network of healthcare facilities, including more than 40 outpatient clinics and six regional hospitals. This comprehensive system provides diverse medical services, covering acute care, specialty care, primary care, mental health services, and preventive dental care for children, among other healthcare offerings. The development process of the survey in this study prioritized content validity, achieved through a rigorous and iterative approach that involved input from a multidisciplinary team comprising researchers, planners, architects, and designers. Furthermore, an exhaustive literature review informed the selection of specific physical environment attributes closely linked with safety perceptions, enhancing the survey’s relevance. It is worth noting that the survey instrument had previously demonstrated its effectiveness in similar projects. However, due to constraints in terms of both budget and time, formal reliability testing for the survey could not be conducted—nevertheless, the robust development process aimed to maximize the survey’s reliability and validity within these limitations.
The survey included demographic questions about age, gender, role, and department. Satisfaction ratings for various physical environment attributes were measured using a Likert-type scale, ranging from 1 (extremely unsatisfied) to 5 (extremely satisfied). Additionally, two optional open-ended questions were included in the online survey to gather deeper understanding of stakeholder’s perceptions:
- How could the physical environment enhance efficiency, experience, or safety?
- What specific changes would you propose to enhance functionality?
The online survey was conducted using Qualtrics and targeted staff members during the study’s early planning and programming stages. It should be noted that formal Institutional Review Board (IRB) approval was not required; however, the survey underwent an internal informal review process. To collect responses, a convenient sampling approach was employed, involving the distribution of the survey to all employees within the healthcare network. This distribution was coordinated internally and took place over three weeks in 2022. While the exact number of employees approached was not disclosed to the research team, it was approximately 2000 individuals. To obtain a representative sample with a 95% confidence level and a 5% margin of error, the target sample size was determined to be around 384 employees. Anonymity was maintained as participants were not required to log in to complete the survey. Data security measures, including encryption and IP address tracking restrictions, were implemented to ensure the protection of participants’ information.
The collected data underwent analysis using descriptive and regression techniques within the Qualtrics XM Stats IQ platform. Descriptive analysis was used to calculate each variable’s frequencies, means, and medians. Regression analysis employed the “Relative Importance” method, recommended for survey data analysis, especially when addressing multicollinearity issues common in survey research. Qualitative insights from open-ended questions were processed using Qualtrics XM Text IQ and Microsoft Excel. Thematic saturation was achieved through a systematic coding process in Qualtrics, where recurring themes were identified and resolved through team discussions. This approach resulted in a comprehensive coding framework covering all identified themes. New responses consistently reinforced existing themes as coding continued, indicating that thematic saturation had been reached. The key themes and findings provided a robust qualitative understanding of the data. A directed content analysis approach was employed to enhance further the depth and comprehensiveness of the analysis, guided by critical safety predictors identified through the regression analysis. The coded results were exported and refined in an Excel document, allowing for additional clustering and analysis, ultimately contributing to a comprehensive qualitative assessment.
Results
Descriptive statistics
This study engaged diverse staff members (n=1,145) with a response rate of approximately 57.25%. Participants ranged from various roles, departments, and age groups, as represented in Figures S1-S3. Descriptive results of staff’s perception of patient and visitor’s satisfaction with physical environment attributes and patient safety are presented in Table 1. Additionally, Table 2 displays the staff’s satisfaction ranking of physical environment components or staff safety.
Table 1
| Variable | n | M | Median |
|---|---|---|---|
| Patient safety | 663 | 3.79 | 4.0 |
| the adjacency of primary rooms in your departments | 514 | 3.38 | 3 |
| Inter-departmental adjacency | 547 | 3.33 | 3 |
| Size of primary rooms | 529 | 3.24 | 3 |
| The flexibility of primary rooms | 517 | 3.23 | 3 |
| Patient privacy | 582 | 3.19 | 3 |
| Reduced patient anxiety | 560 | 3.13 | 3 |
| Wayfinding | 597 | 3.08 | 3 |
| Comfortable furniture | 609 | 3.07 | 3 |
| Clear signage | 616 | 3.05 | 3 |
| Convenient parking access | 599 | 3.03 | 3 |
| Family privacy | 554 | 3.03 | 3 |
| Access to daylighting | 583 | 3.01 | 3 |
| Positive distractions | 577 | 3.00 | 3 |
| Views to nature | 578 | 2.97 | 3 |
| Storage space for personal belongings | 544 | 2.95 | 3 |
| Cleanliness | 611 | 2.94 | 3 |
| Acoustical levels | 594 | 2.93 | 3 |
| Attractive or inviting colors or materials | 604 | 2.84 | 3 |
| Quality of flooring | 604 | 2.84 | 3 |
Table 2
| Variable | Count | Average | Median |
|---|---|---|---|
| Staff safety | 781 | 3.68 | 4.0 |
| Security | 779 | 3.61 | 4.0 |
| Visual display of work information | 770 | 3.53 | 4.0 |
| Proximity of supplies | 769 | 3.52 | 4.0 |
| Team visibility | 760 | 3.45 | 4.0 |
| Patient visibility | 651 | 3.43 | 3.0 |
| Department adjacency | 711 | 3.39 | 3.0 |
| The adjacency of primary rooms in your departments | 680 | 3.33 | 3.0 |
| Number of equipment | 745 | 3.29 | 3.0 |
| Equipment quality | 760 | 3.26 | 3.0 |
| Convenient parking access | 766 | 3.21 | 3.0 |
| Department size | 789 | 3.20 | 3.0 |
| The flexibility of primary rooms | 645 | 3.20 | 3.0 |
| Number of primary rooms in your department | 696 | 3.16 | 3.0 |
| Number of radiology room | 297 | 3.15 | 3.0 |
| Size of primary rooms in your department | 701 | 3.14 | 3.0 |
| Number of exam rooms | 510 | 3.12 | 3.0 |
| Adequate team collaboration spaces | 763 | 3.09 | 3.0 |
| Staff workspace size | 784 | 3.08 | 3.0 |
| Comfortable furniture | 775 | 3.04 | 3.0 |
| Number of staff office spaces | 741 | 3.01 | 3.0 |
| Quality of staff office spaces | 746 | 3.01 | 3.0 |
| Staff privacy | 780 | 2.94 | 3.0 |
| Cleanliness | 792 | 2.91 | 3.0 |
| Acoustical levels | 751 | 2.87 | 3.0 |
| Access to daylighting | 768 | 2.84 | 3.0 |
| HVAC performance | 735 | 2.83 | 3.0 |
| Adequate staff break rooms | 760 | 2.83 | 3.0 |
| Attractive or inviting colors or materials | 764 | 2.76 | 3.0 |
| Views to nature | 745 | 2.71 | 3.0 |
| Quality of flooring | 777 | 2.67 | 3.0 |
| Storage space | 761 | 2.67 | 2.0 |
HVAC, heating, ventilation and air conditioning.
Regression modeling
The regression model assessed staff perceptions of patient and visitor safety, incorporating the variables outlined in Table 1. The results, as presented in Table 3, indicate that patient privacy, space adjacency, positive distraction, clear signage, cleanliness, and flooring quality emerged as significant predictors for satisfactory patient and visitor safety [n=663, adjusted R-squared =23.1%, standard error (SE) =0.879, P<0.00001]. Furthermore, it is noteworthy that staff’s perception of patient or family satisfaction with privacy and room adjacency accounted for 23% of staff satisfaction with patient safety perceptions, suggesting that while these factors play a substantial role, other unexplored variables may influence safety perceptions.
Table 3
| Variable | Relative importance | Coefficient | P value | Imputed value |
|---|---|---|---|---|
| Patient privacy | 23.2% | 0.117242 | <0.0001 | 3.194158 |
| Adjacency of primary rooms in departments | 23.1% | 0.156262 | <0.00001 | 3 |
| Positive distractions | 20.0% | 0.125862 | 0.004197 | 3.001733 |
| Clear signage | 17.0% | 0.10012 | 0.021772 | 3.051948 |
| Cleanliness | 12.5% | 0.075029 | 0.004883 | 2.944354 |
| Quality of flooring | 4.0% | 0.029406 | 0.011879 | 2.836093 |
Additionally, the regression model evaluating satisfaction with staff safety perceptions included all variables detailed in Table 2. As indicated in Table 4, the relative importance regression analysis identified several significant predictors: security, staff privacy, team visibility, and comfortable furniture (n=781, adjusted R square =46.6%, SE =0.823, P<0.00001). These findings underscore the multifaceted nature of staff safety perceptions within healthcare environments and emphasize the importance of various factors in shaping these perceptions.
Table 4
| Variable | Relative importance | Coefficient | P value | Imputed value |
|---|---|---|---|---|
| Security | 49.7% | 0.230911 | <0.00001 | 3.612323 |
| Staff privacy | 24.5% | 0.138648 | <0.00001 | 2.935897 |
| Team visibility | 15.1% | 0.106837 | 0.000473 | 4 |
| Comfortable furniture | 10.7% | 0.084569 | 0.00607 | 3.042581 |
Open-ended comments
In our study, we collected insights from 393 respondents regarding potential improvements to the physical environment, focusing on enhancing team efficiency and patient safety (Question 1). Furthermore, 433 staff members shared insights specific to their respective departments (Question 2). Given that two separate questions were employed, which resulted in varying participant counts, it was necessary to combine these responses to gain a deeper understanding of the emerging themes. From the analysis of open-ended responses, we identified a total of fourteen themes related to physical environment attributes that have an impact on safety perceptions. Table 5 illustrates the quantity and examples of staff quotes relevant to the extracted themes. The results revealed that there was an overlap between individuals who provided department-specific and generalized feedback, as a portion of respondents offered both department-specific and generalized feedback. This overlap suggests that some participants shared broader insights while also providing input specific to their departments. However, it is important to note that most respondents tended to focus on either department-specific or generalized feedback, with only a smaller subset offering both.
Table 5
| Theme | Code | Impact on safety |
|---|---|---|
| Patient privacy (n=145) | Patient acoustical privacy, private rooms, private bathroom, HIPAA compliance | “There is no privacy for us to check in patients for appointments, and there are constant HIPAA violations because of the design of the office.” |
| “Private rooms for inpatients would be better due to patient privacy and infection control.” | ||
| “Rooms have no soundproofing, and conversations can easily be overheard.” | ||
| Cleanliness (n=131) | Cleanliness of the overall environment, floors, rooms, curtains, surfaces, bathrooms, and patient rooms | “Painted walls, floors without damage, dirt, and dust, and clean windows all work to make the patient safe and feeling safe and comfortable.” |
| “Our building is never cleaned. We have bags of trash in breakrooms and sometimes in the halls. The bathrooms are disgusting, toilets are not cleaned, and trash is overflowing.” | ||
| “The flooring has been terrible. Most mornings, we open the clinic to dirty floors that have not been cleaned, trash not removed, and roaming herds of dust bunnies. We are performing procedures, and the rooms are not clean.” | ||
| Staff privacy (n=36) | Acoustical privacy for virtual meetings or team meetings | “Perioperative care - there is no glass barrier shielding conversations from patients regardless of having to monitor patients - communication should still be private as discussions include pertinent patient information.” |
| “Walls too thin. Patients can hear what is said in adjacent exam rooms/offices/nurses’ stations. Very little privacy.” | ||
| Floor type (n=33) | Removing floors, repairing floors, removing carpet | “Better flooring would mean fewer trips/slips, as well as safer from an infection control standpoint over the current carpeting.” |
| “Clean/new carpet and painting walls would provide a bright, clean environment and reduce allergens from old dirty carpet.” | ||
| “It is great that the carpeting has been taken up and tile is put in its place in the clinic area. Carpeting should not be in the clinics at all. It cannot be thoroughly cleaned & holds allergens, dust & other unhealthy things.” | ||
| Ergonomics (n=32) | Furniture or equipment ergonomics | “Chairs at nurse station desks are ripping and unsafe.” |
| “Access to equipment that would make the job more ergonomic is often denied (standing desk, headsets, wrist/mouse rests for hands, etc.).” | ||
| “The office chairs are aged, dirty, and uncomfortable.” | ||
| Visual connectivity (n=28) | Openness, visual connectivity | “Patient room doors with windows to view the patients would allow us to visualize the patients and thereby increase patient safety.” |
| “If we could see [inside] all the patient rooms, we would be more aware of what was happening immediately.” | ||
| Room size (n=23) | Needing more space, crowded environments | “With a larger space and better workflow, it reduces the likelihood of an error, which improves patient safety and tends to be quicker with enhancing the patient experience.” |
| “More open space in outpatient clinics would mean fewer safety issues related to poor space issues. It would allow staff to expand their practices and include interventions that currently we cannot pursue due to space limitations.” | ||
| “In one location, patients have tripped, fallen, and been injured secondary to insufficient space to adequately house large pieces of equipment or staff workstations being in the walkway between areas in the clinic.” | ||
| Security (n=19) | Patient violence, distance to security staff | “Staff is positioned at the far end of the treatment room, so if a patient becomes violent or threatening, staff has to pass them to exit.” |
| “Perhaps one or two closed circuit cameras or change the entrance so we can see who is coming in if they have fallen/need assistance or have a weapon. Front staff cannot see who has entered until they are a foot from them.” | ||
| Programming (n=18) | Spatial adjacency, med rooms, dirty utility, clean room | “We should have one floor; we have an elevator that is broken down more than it works, so patients have to go back to their cars and drive around to the back of the building or vice versa, which is not safe for the elderly, especially in the winter months.” |
| “A dedicated med room that locks to improve safety and patient flow.” | ||
| “We currently have crutches and walkers to give to patients stored in the dirty utility room, which is not sanitary.” | ||
| Code compliance (n=14) | Fire distinguishers, sprinkler system, the path of egress | “Our current building has been out of compliance since 2015 with expired fire extinguishers lasted services back in 2015. We also have missing smoke detectors, no breakroom, and no privacy to meet with the patients as needed.” |
| “We MUST change the way the bathroom doors open in rooms 516 and 517 - they should open INTO the bathroom, not into the patient room. This [lack of clearance] is a MAJOR safety hazard for both patients and staff.” | ||
| Technology-equipment (n=12) | Trip hazard, access control | “Our bedside computers are cumbersome and dangerous d/t always coming unhinged, falling sideways, so the scanner can fall off the side and break.” |
| “To enhance staff safety, there should be a keypad or badge tap to enter the hallway where the lab is.” | ||
| Layout properties (n=11) | Sinks, therapeutic experience, central nurse stations | “Mental health providers should have more comforting rooms and less clinical. Currently, they see patients in an exam room with an exam table, uncomfortable chairs, and no art. This is not conducive to helping patients with their anxiety or helping them feel safe to talk about their issues.” |
| “If all nurses were in 1 nurses’ station, Rooming of patients becomes timelier and more efficient, resulting in an improved and satisfying patient experience, and enhanced patient safety as delays should be minimal if any.” | ||
| Environmental conditions (n=5) | HVAC, lighting | “There is inadequate ventilation to meet with patients during covid safely, and the portable HEPA filters make too much noise to run during patient appointments.” |
| “Upgrade lighting in SPD (safety and infection control) improve staff ability to visualize instrument processing problems.” | ||
| Signage (n=17) | Signage and wayfinding | “The wayfinding, signage, and distance traveled to the exam room for our elderly patients is suboptimal.” |
| “Color floor tiles or clearer signage to help direct patients to the correct registration desk or exit.” | ||
| “Paint and update décor- improve the department’s mood for patients and staff.” | ||
| Team visibility (n=6) | “Ability to communicate with secretaries and providers, able to keep an eye out for patients.” | |
| “Managers and Supervisors to be in one area for ease of communication.” | ||
| Positive distraction (n=114) | View of nature, artwork, colors | “With the right-sized curtains and clean windows, the patient can experience quicker healing with views of nature and more control over the glaring sun.” |
| “This clinic has no views of nature (or windows, for that matter).” | ||
| “The view is of a smokestack on a black rubber roof. The artwork is sun-bleached.” |
HIPAA, Health Information Portability and Accountability Act; HVAC, heating, ventilation and air conditioning; SPD, surge protective services.
In applying the directed content analysis approach, we intentionally included specific themes such as signage, positive distraction, and team visibility in Table 5, even though these elements were not explicitly mentioned by respondents as direct contributors to their safety perceptions. Furthermore, it’s noteworthy that the participants placed emphasis on factors like code compliance, technology and equipment, visual connectivity with patients, and room size in relation to safety perceptions, despite these aspects not being identified as significant predictors in the regression model. The inclusion of this information in Table 5 is intended to provide a foundation for potential areas of research exploration in the future.
Table 6 summarizes how staff connected improved safety conditions to various related perceptions. This paper will delve into comments on the significant regression predictors, which will be highlighted in the subsequent sections. The counts (n) represent the number of coded responses for each theme. The variation in the counts reflects the diversity in participants’ responses, rather than implying the relative importance of themes. It is important to emphasize that the numbers are not indicative of the significance of a theme but rather demonstrate the prevalence of certain topics within the data. The wide range is a result of the participants’ diverse perspectives and the richness of the qualitative data. Each theme contributes uniquely to our understanding of the subject matter, and none should be perceived as less important than others. Our intention is to provide a comprehensive overview of the various aspects raised by the participants in their feedback.
Table 6
| Improved safety outcomes | n | % |
|---|---|---|
| Reduced falls | 13 | 23% |
| Improved infection control | 13 | 23% |
| Improved staff and patient experience | 11 | 19% |
| Improved delivery of care | 7 | 12% |
| Efficiency and cost | 6 | 11% |
| Improved staff physical health | 5 | 9% |
| Staff satisfaction | 1 | 2% |
| Improved space usage | 1 | 2% |
| Sum | 57 | 100% |
Patient privacy
Patient privacy was identified as a critical factor in enhancing patient safety perceptions (n=145). Participants recommended various physical environment features to improve patient privacy, including private patient rooms, reconfigured furniture, sound-absorbing materials, wall divisions, and improved spatial design in registration and check-out areas. Staff members emphasized the importance of acoustically designed spaces in supporting HIPAA guidelines and improving the patient experience while reducing staff anxiety, particularly in patient rooms and registration areas. Furthermore, specific spaces, such as the therapy gym, were reported to have inadequate sizes that compromised patient privacy. The limited space resulted in a noisy environment, making it challenging for patients to follow directions and participate effectively in physically demanding activities.
Staff privacy
Participants highlighted the significance of workspaces that ensure acoustical privacy for staff members (n=25). Shared offices with staff engaged in frequent virtual calls posed challenges, as private conversations could be overheard due to limited space. This compromised staff focus and violated HIPAA policies. Nurses recommended potential solutions such as incorporating soft music or white noise in the environment and utilizing plastic windows around nurse stations. Enhancing privacy at the nurses’ station and implementing noise machines in patient rooms were also suggested to minimize the audibility of sensitive conversations and phone calls.
Space planning
Based on feedback from 80 participants, the study identified the improvement of spatial adjacencies as a crucial aspect of healthcare facility design. Participants emphasized the need for better spatial adjacency and accessibility to address patient and visitor frustration, inadequate patient privacy, and the risk of falls for elderly patients, particularly in winter. Insufficient parking near healthcare facilities negatively affected the patient’s experience, causing frustration and delays. Inefficient adjacencies posed significant challenges, especially for the elderly, who had to navigate long distances that were deemed unsafe, particularly during winter months.
Participants highlighted the importance of departmental adjacency and access for achieving positive patient safety perceptions. Inadequate adjacencies adversely affected patient wayfinding experience and throughput perceptions. For instance, staff members reported confusion and workflow/patient throughput issues arising from the shared space between the dentist’s front desk and the therapy front desk. A nurse in the inpatient birthing center emphasized the need for a dedicated floor to ensure infant safety, which would improve travel patterns, patient satisfaction, and overall infant safety.
The absence of necessary space functions adjacent to or within a department had a detrimental impact on travel distances, patient experience, and safety perceptions. Staff members in the birth center highlighted how the lack of operating rooms (ORs) in their unit compromised patient safety. Moreover, the unit’s size and the spaces’ adjacency influenced travel distances and staff assignments. Participants raised concerns about the safety risks of long walking distances between departments. Lastly, the lack of acoustical privacy and patients traversing provider office areas during appointments were identified as violations of HIPAA guidelines. Staff members reported being able to hear dictations, compromising patient privacy and safety.
Cleanliness
The cleanliness of healthcare spaces was identified as critical for ensuring patient and staff safety by minimizing the risk of infection transmission and allergen-related issues (n=131). Staff members recommended implementing regular cleaning and dusting practices for floors, exam rooms, offices, bathrooms, trays, and linen to maintain sanitary conditions. Concerns were raised regarding the need for sufficient housekeeping staff, leading some staff members to clean the spaces themselves. Nurses in the ED highlighted limited cleaning assistance at night, which only covered specific areas upon request. Dusting surfaces was emphasized as essential for promoting staff safety and health, as dust can aggravate allergies. Staff members suggested removing carpets, improving environmental brightness, and reducing allergen exposure.
Quality of flooring
Insights from a subset of participants (n=33) highlighted the critical role of flooring quality in influencing safety perceptions. The type of flooring was observed to impact its cleanability and potential to harbor pathogens. Staff members recommended replacing carpet flooring with impermeable materials like sheet vinyl or epoxy flooring to enhance infection control and maintain cleanliness. Additionally, the influence of flooring types, particularly carpets, on the presence of tripping hazards was noted.
Security
Adequate technology and staffing were crucial factors in creating a secure environment and ensuring the staff’s sense of safety. Staff members raised security concerns, particularly in surgery, registration, outpatient clinics, and EDs (n=19). Insufficient or absent security personnel resulted in verbal abuse from patients, leading to an insecure environment. Participants recommended implementing physical changes, such as improved ambient conditions through adequate lighting in the ED, to mitigate visitor hostility. Design modifications, including safe and easily accessible exits from each department, were deemed necessary for emergent events. Suggestions were made to enhance security systems, such as closed-circuit cameras at entrances and exits and lockable inter-department doors with key-badge access.
Team visibility
A small group of participants emphasized the importance of team visibility in ensuring staff safety (n=6). Proximity among staff members was critical for improving awareness of potential safety issues and enabling timely emergency responses. Team visibility was also seen as a deterrent against violence or aggression towards staff. Staff working in isolated or separate areas perceived a higher risk of such incidents. Recommendations included locating nurses and administrative staff near enhanced team visibility for improved access and communication and identifying segmented floor plans that hinder effective team collaboration and care delivery.
Ergonomic furniture and equipment
The importance of ergonomic, clean, and comfortable furniture and equipment for promoting staff health and safety was highlighted by participants (n=15). Ergonomic equipment was seen to reduce physical strain on healthcare providers during direct patient care. Suggestions included providing adjustable exam tables and ceiling lifts, particularly for transferring bariatric patients.
Positive distraction
Staff members highlighted the importance of incorporating positive distractions and enhancing aesthetics in healthcare facilities (n=114). They believed these measures could significantly improve patients’ experiences, create a therapeutic and safe environment, increase comfort levels, enhance satisfaction, and boost staff morale. One staff member mentioned that patients desired more windows, allowing access to natural light and providing views of therapeutic scenery. Additionally, staff members recommended utilizing bright and cheerful colors in pediatric environments as an effective strategy to distract patients and reduce their stress levels.
Signage
According to feedback from 17 participants, effective signage emerged as a crucial attribute for enhancing patient flow, efficiency, and experience. An excessive number of signs were found to overwhelm patients. However, it was emphasized that the quantity and placement of signage should be strategically determined to minimize confusion and enhance visibility. Clear and prominently displayed signage was important for wayfinding across various departments, floors, exits, and entrances. A staff member from the imaging department highlighted the necessity for clearer signage or color-coded floor tiles to guide patients back to the main entrance. Participants further recommended the deployment of volunteer staff to assist patients that encounter difficulties with wayfinding due to inadequate signage.
Discussion
Comparison with similar research
The study’s comprehensive findings, drawing from quantitative and qualitative data, provide essential insights into enhancing safety through healthcare facility design, aligning well with the JDCS model principles. While our strategic plan set overarching objectives, the survey results empowered our team to create customized, evidence-based solutions tailored to individual departments and sites, a user-centric approach consistent with the JDCS model’s focus on job characteristics and employee well-being (68,69).
This approach was instrumental in bridging the gap between leadership goals and staff needs, akin to how the JDCS model addresses the interplay between job demands, control, and social support in the workplace (69). Collecting and incorporating end-user feedback right from the outset enriched our facility planning process, resulting in master plans deeply rooted in the realities of daily operations and direct patient care. In the subsequent sections, we will further explore the relationship between significant predictors of safety perceptions, draw parallels with related research, and dissect their implications within our facility planning process, all within the context of the JDCS model’s principles.
Patient privacy
The study’s findings align closely with existing literature on the importance of patient privacy in healthcare facility design (8,12-15). Recommendations such as the introduction of private patient rooms, sound-absorbing materials, and improved spatial design for registration and check-out locations reflect the significance of these factors in healthcare facility planning, reinforcing their relevance (8,13-15).
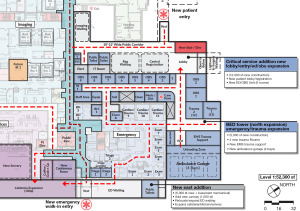
Additionally, the study’s revelation regarding inadequate space sizes compromising patient privacy underscores an underexplored aspect of healthcare design. This new knowledge led to our adaptations in planning and design processes that emphasized individual patient rooms and strategic workstation and registration area placements (Figure 1). These modifications were made with the dual purpose of improving sound isolation and placing a high priority on enhancing the patient’s experience by upholding privacy as a fundamental element of healthcare environments. Future research opportunities lie in quantitatively measuring the impact of specific design changes on patient privacy perceptions, such as private patient rooms and sound-absorbing materials. By prioritizing patient privacy through thoughtful spatial planning, healthcare organizations and policymakers create environments that comply with existing regulations and enhance patient experience and safety.

Staff privacy
In alignment with previous research on staff privacy in healthcare settings (13,14,17,19-21), prioritizing acoustical privacy emerges as a fundamental aspect not only for enhancing staff satisfaction but also for promoting staff safety and improving overall patient care quality, as substantiated by our findings. This parallels existing literature highlighting the significance of utilizing sound-absorbing materials, such as acoustic panels and wall treatments, particularly in open-plan work environments, to mitigate noise and enhance privacy (70-72).
However, expanding our perspective on this finding is essential, considering its implications for clinical staff perceptions of staff privacy and safety. The absence of acoustical privacy becomes a latent factor that may lead to situations where clinical staff can be overheard, potentially triggering stress in families and visitors, which could result in aggression towards staff and subsequently reduce the staff’s sense of safety. This complex interplay emphasizes the need for further research to delve into the multifaceted dynamics between acoustical privacy, staff safety, and overall healthcare quality.
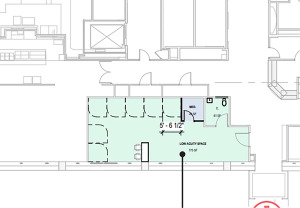
Considering these findings, our planning approach incorporated customized interventions to address these concerns, including establishing staff-exclusive zones, dedicated workstations, private offices, and limited access staff corridors (Figure 2). From a policy perspective, our research underscores the necessity for healthcare facility design guidelines and standards to include recommendations for soundproofing measures, appropriate room layouts, and technology enhancements to ensure audio privacy, especially in spaces designated for telemedicine. Integrating evidence-based design principles can significantly create healthcare environments prioritizing staff well-being and patient safety.

Space planning
The study’s findings corroborate the substantial impact of efficient spatial planning on both staff and patient safety, aligning with prior research emphasizing the significance of factors like spatial adjacency and wayfinding in healthcare facility design (3,6,9,13,25,26,30,31). Notably, participants in the current study recognized the pressing need for improved spatial adjacency and accessibility, acknowledging their potential to alleviate patient and visitor frustration, enhance patient privacy, and reduce the risk of falls. These insights prompted significant changes in our facility design approach.
In direct response to these valuable insights, we initiated the strategic relocation of several departments within the healthcare facility layout to minimize staff walking distances and improve access (Figures 3,4). Through this approach, we sought to mitigate factors contributing to staff fatigue, stress, and susceptibility to interruptions, all of which have direct implications for patient safety, as supported by prior research (27-29). Furthermore, our facility design incorporated various interventions, including improved parking adjacency (Figure 5) and enhanced visibility to entrances that have been found as wayfinding solutions in mitigating stress, patient absenteeism, late arrivals, and frustration (13,45,73).


However, despite the progress in understanding the link between spatial planning and safety perceptions, a significant knowledge gap still needs to be addressed. Future research is recommended to explore specific dimensions and design elements that optimize spatial adjacency and wayfinding within healthcare facilities. Additionally, assessing the long-term impact of these design changes on staff and patient safety and overall well-being could provide further insights into the effectiveness of such interventions, contributing to the ongoing improvement of healthcare facility design and its impact on safety.
Cleanliness
Our study’s findings align seamlessly with existing literature, emphasizing the crucial role of improved cleaning and disinfection protocols in decreasing patient infection rates—a concern that resonated significantly among our staff participants (10,32,33,35,74). This correlation underscores the significance of upholding cleanliness standards in healthcare environments to mitigate the risks associated with infection transmission and allergen-related issues. Additionally, our staff participants acknowledged the importance of flooring material choices and safety, a topic that has been thoroughly explored in previous research (39,75).
Considering these findings, our planning recommendations include replacing carpet flooring with impermeable materials such as sheet vinyl or epoxy flooring, aligning with the knowledge that flooring materials can significantly impact cleanliness and safety. To bridge the current knowledge gap, future research should delve deeper into specific cleaning and disinfection protocols and practices most effective in minimizing infection risks within healthcare environments. Additionally, exploring the long-term effects of flooring material choices on cleanliness, pathogen growth, and safety outcomes would provide valuable insights for healthcare facility planners and policymakers. This research can contribute to the ongoing enhancement of infection control strategies and the design of healthcare facilities, ultimately ensuring patients’ and staff’s safety and well-being.
Quality of flooring
The perceptions of our staff participants align with established literature, highlighting the significant influence of flooring quality on falls, gait, and the severity of injuries (39,41,76-78). These insights underscore the importance of carefully selecting shock-absorbing flooring materials such as carpet, wood, or linoleum sheets when planning healthcare facilities in accordance with prior research recommendations (39,76,77). In response to these findings, our planning team has proposed incorporating appropriate flooring materials, explicitly focusing on mitigating pathogen growth, reducing tripping hazards, and preventing fall-related injuries within healthcare settings. By integrating these flooring materials into the facility design, we aimed to create safer healthcare environments that prioritize the well-being of both patients and staff.
To address the current knowledge gap, future research should delve into the long-term effects of flooring material choices on falls, injury rates, and overall safety outcomes in various healthcare contexts and among different patient populations. This research could offer valuable insights into the optimal flooring solutions and their implications. From a policy perspective, guidelines should consider the shock-absorbing properties of flooring materials and their potential impact on pathogen control and patient safety, ensuring a comprehensive approach to healthcare facility planning and design.
Security
Staff perception of security’s impact on staff safety aligns with extensive research findings (13,23,45-47). Furthermore, our study aligns with prior evidence (13,23,45,47,49), as staff identified several crucial design components within the physical environment that have the potential to enhance security perceptions significantly. These identified components include well-planned lighting and easily accessible exits, essential considerations during the facility planning phase to bolster security measures.
To proactively enhance security during the facility planning, we implemented targeted interventions, as depicted in Figure 6. These interventions included initiatives such as improving the visibility of entrance and exit doors for registration and security personnel, establishing dedicated security personnel stations within the ED, designating staff-exclusive corridors, implementing badge access systems, and strategically optimizing the proximity of security stations to various departments. By integrating these specific measures into the facility’s design, we aim to create a healthcare environment that is safer and more secure, ultimately benefiting both staff and patients.

Team visibility
The findings of this study align closely with prior research emphasizing the critical role of team visibility in promoting staff safety and collaboration (5,23,24,49,51). To incorporate these insights into our facility planning process, we prioritized specific design strategies, including open layouts, wider corridors, and the strategic placement of nurse stations or security stations, all of which have strong support in the literature for enhancing team visibility within healthcare facilities (5,13,23,24,49,53). Nevertheless, as highlighted by Naccarella (24), our approach aimed to strike a balance between open workspaces that enhance team visibility and communication and the provision of adequate spaces for private conversations.
However, it is essential to note a limitation of this study: the relatively small sample size of participants that emphasized the importance of team visibility in their safety perceptions. While these findings provide valuable insights, future research with more extensive and diverse samples could further validate and expand upon these observations. To drive improvements in healthcare facility design, policymakers, and healthcare administrators should consider incorporating design elements that facilitate team visibility, such as open layouts, wider corridors, and strategically located nurse or security stations, into guidelines and standards for healthcare facility construction and renovation. These measures hold the potential to significantly contribute to creating safer and more collaborative healthcare environments for both staff and patients, ultimately enhancing the quality of care provided.
Comfortable furniture and equipment
This finding aligns with prior research emphasizing the critical role of comfortable furniture in enhancing staff health and safety (54-57,79). Facility planners utilized this insight as a valuable reference point during their collaborative efforts with interior designers, healthcare administrators, and policymakers. While overall equipment satisfaction may not have emerged as a significant predictor of staff safety in the regression model, open-ended comments from studies highlight the substantial impact of equipment ergonomics on reducing the risk of WMSDs, aligning with prior research (57-60). Ergonomics training has been recommended to educate staff on WMSD risk factors and how ergonomics can enhance their work’s ease, efficiency, and safety (58,59).
Indeed, while overall equipment satisfaction may not have directly predicted staff safety satisfaction, it is crucial to underscore the literature’s consistent emphasis on the importance of ergonomically designed equipment in safeguarding staff musculoskeletal health and preventing WMSDs. Future research in the realm of design should delve into the specific ergonomic features and design principles that contribute most effectively to staff musculoskeletal health and safety. This could include in-depth studies on the impact of ergonomically designed furniture, equipment layout, and workstation configurations on reducing the risk of WMSDs among healthcare staff. Such research could provide actionable insights for interior designers and policymakers to create healthcare environments prioritizing staff comfort, health, and safety, ultimately enhancing the quality of care.
Positive distraction
The regression analysis findings highlight the significance of positive distractions, a concept well-supported by prior research in healthcare settings (61-66). This alignment with existing research underscores the importance of integrating positive distractions into healthcare facility design and management to enhance overall well-being and safety (61,62,66). However, it is paramount to note that the open-ended comments from our study did not directly establish a connection between positive distractions and safety perceptions. This suggests a potential gap in understanding the latent variable of positive distraction and its impact on satisfaction with patient and visitor safety. Addressing this gap in future research can provide deeper insights into the relationship between positive distractions and safety perceptions, further informing healthcare facility design strategies to improve safety outcomes. During the planning phase, we prioritized patient rooms and waiting areas along exterior walls to ensure access to natural daylight and outdoor views (Figure 7). We also undertook room reconfigurations to ensure sufficient space to accommodate staff and patient requirements.
Signage
The findings of our study resonate with the existing literature that underscores the importance of clear and efficient signage in healthcare settings to enhance wayfinding (13,31,80). This alignment with prior research highlights the need to balance the quantity and placement of signage, a recommendation consistently supported by previous studies (80). Although the immediate implications of signage were not initially incorporated into our initial planning efforts, they were identified as a crucial objective for our client’s future development plans. The potential integration of these findings into healthcare facility design and planning processes offers a promising area for future research. There is a need for more comprehensive investigations to explore the specific design characteristics and features of signage that have the most significant impact on wayfinding efficiency and safety perceptions. These findings emphasize the importance of healthcare policymakers and facility planners prioritizing efficient spatial planning and wayfinding solutions. By doing so, healthcare organizations can enhance safety and improve the overall experience for staff and patients.
Key findings
This study reaffirms the well-established understanding that the design of the physical environment in healthcare settings substantially impacts staff safety perceptions. Our research identified critical factors influencing perceptions of patient and visitor safety for staff, including patient privacy, spatial adjacency, positive distractions, clear signage, cleanliness, and flooring quality. Furthermore, satisfaction with staff safety was significantly predicted by factors such as security, staff privacy, team visibility, and the presence of comfortable furniture. In addition to confirming existing knowledge, this research unveils novel insights by highlighting previously overlooked elements in the physical environment, including positive distractions, spatial layout, signage, and comfortable furniture, as significant predictors of staff satisfaction regarding safety perceptions.
Strengths and limitations
The study boasts several strengths. Firstly, it employed a holistic approach by gathering quantitative and qualitative data, providing a comprehensive understanding of the relationship between healthcare facility design and safety perceptions. Additionally, the study’s strength lies in its diverse participant pool, incorporating insights from various stakeholders such as clinical staff, non-clinical staff, and administrators, enhancing the generalizability of the findings. Moreover, the study contributes to existing knowledge by pinpointing previously overlooked factors, like positive distractions, staff privacy, or spatial planning, as significant predictors of staff satisfaction regarding safety perceptions. Finally, another strength of this study lies in its practical implications. The identified key drivers of safety perceptions offer actionable insights for healthcare organizations, architects, designers, and policymakers. Prioritizing patient privacy, spatial layout, positive distractions, clear signage, cleanliness, security, and ergonomic furniture can optimize healthcare environments for safety and well-being.
Nevertheless, it is crucial to recognize the study’s limitations. One notable constraint is the relatively small sample size for specific emerging themes, potentially limiting the broader applicability of the findings. To enhance the robustness of these perceptions, future research should aim for more extensive and diverse participant pools. Moreover, while the study identified significant predictors of safety perceptions, it still needed to explore the causal relationships between these factors and actual safety outcomes. In this regard, further research is warranted to investigate the mechanisms through which healthcare facility design influences safety perceptions and concrete safety results. Another area for improvement lies in focusing solely on staff perceptions; the research team could not collect data from patients or visitors regarding their safety perceptions. This restricts the study’s scope to staff perspectives and leaves room for future studies to encompass a more comprehensive view of safety perceptions in healthcare settings.
During our research, we have underscored the paramount importance of designing clear, concise, and comprehensive surveys, recognizing their pivotal role in soliciting feedback from stakeholders and the consequential impact on the quality of the acquired data. In forthcoming facility planning endeavors, we intend to translate these insights into practice by meticulously crafting surveys that are adept at capturing a broad spectrum of perspectives, with a specific emphasis on distinct stakeholder categories including staff, patients, and management. Furthermore, we have gained an appreciation for the added depth and breadth that can be achieved by considering a wider array of participant characteristics in surveys, such as their professional roles. This heightened understanding of the varied perspectives and needs of diverse stakeholders has been a fundamental component of our future surveys, especially in the realm of master facility planning. This practice becomes particularly pertinent as different roles and departments assume discrete responsibilities in the overarching planning and design of healthcare facilities.
Conclusions
In summary, this study comprehensively explains the intricate relationship between healthcare facility design and staff perceptions of safety. Employing a user-centered approach and utilizing quantitative and qualitative research methods, this research has paved the way for tailored, evidence-based solutions bridging the gap between leadership priorities and staff requirements. The findings resonate with existing literature, reaffirming the importance of various design elements in healthcare environments. Utilizing a user-centered approach and quantitative and qualitative research methods, the research provides evidence-based solutions aligning leadership priorities with staff needs. Emphasizing the significance of design elements in healthcare environments, the findings reinforce existing literature and advocate for enhancements such as private rooms, sound-absorbing materials, and acoustical privacy measures. The findings underscore the importance of positive distractions, spatial planning, team visibility, and ergonomic furniture in promoting staff perceptions of safety. In summary, we emphasize the importance of integrating these physical environment qualities into future facility planning and policy development, with the goal of creating safer, more patient-centered, and efficient healthcare environments.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-93/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-93/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-93/coif). All authors are members of a BSA LifeStructures team that has entered into a contract with the Bassett Healthcare Network. The team is tasked with designing and suggesting modifications for current healthcare facilities. All authors report support for attending meetings from Bassett Hospital. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. There is no need of IRB approval as patients were not involved. Anonymity was maintained as participants were not required to log in to complete the survey. Data security measures, including encryption and IP address tracking restrictions, were implemented to ensure the protection of participants’ information.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Patient Safety: Global Action on Patient Safety. 72nd World Health Assembly. [Internet]. 2021 [cited 2023 Apr 4]. Available online: https://www.who.int/westernpacific/health-topics/patient-safety
- Agency for Healthcare Research and Quality. Patient safety primer: Patient safety [Internet]. 2022 [cited 2023 May 8]. Available online: https://www.ahrq.gov/patient-safety/about/index.html#:~:text=AHRQ%20is%20the%20lead%20federal,health%20care%20that%20reaches%20patients
- Garcia CL, Abreu LC, Ramos JLS, et al. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina (Kaunas) 2019;55:553. [Crossref] [PubMed]
- Lundin S. Can Healing Architecture Increase Safety in the Design of Psychiatric Wards? HERD 2021;14:106-17. [Crossref] [PubMed]
- Pati D, Harvey TE Jr, Pati S. Physical design correlates of efficiency and safety in emergency departments: a qualitative examination. Crit Care Nurs Q 2014;37:299-316. [Crossref] [PubMed]
- Al Ma'mari Q, Sharour LA, Al Omari O. Fatigue, burnout, work environment, workload and perceived patient safety culture among critical care nurses. Br J Nurs 2020;29:28-34. [Crossref] [PubMed]
- Robakowska M, Bronk M, Tyrańska-Fobke A, et al. Patient Safety Related to Microbiological Contamination of the Environment of a Multi-Profile Clinical Hospital. Int J Environ Res Public Health 2021;18:3844. [Crossref] [PubMed]
- Shen N, Bernier T, Sequeira L, et al. Understanding the patient privacy perspective on health information exchange: A systematic review. Int J Med Inform 2019;125:1-12. [Crossref] [PubMed]
- Chaudhury H, Mahmood A, Valente M. The effect of environmental design on reducing nursing errors and increasing efficiency in acute care settings: a review and analysis of the literature. Environ Behav 2009;41:755-86. [Crossref]
- Assadian O, Harbarth S, Vos M, et al. Practical recommendations for routine cleaning and disinfection procedures in healthcare institutions: a narrative review. J Hosp Infect 2021;113:104-14. [Crossref] [PubMed]
- Strini V, Schiavolin R, Prendin A. Fall Risk Assessment Scales: A Systematic Literature Review. Nurs Rep 2021;11:430-43. [Crossref] [PubMed]
- Pullmann MD, VanHooser S, Hoffman C, et al. Barriers to and supports of family participation in a rural system of care for children with serious emotional problems. Community Ment Health J 2010;46:211-20. [Crossref] [PubMed]
- Zamani Z. Effects of Emergency Department Physical Design Elements on Security, Wayfinding, Visibility, Privacy, and Efficiency and Its Implications on Staff Satisfaction and Performance. HERD 2019;12:72-88. [Crossref] [PubMed]
- Olsen JC, Sabin BR. Emergency Department patient perceptions of privacy and confidentiality. J Emerg Med 2003;25:329-33. [Crossref] [PubMed]
- Lin YK, Lee WC, Kuo LC, et al. Building an ethical environment improves patient privacy and satisfaction in the crowded emergency department: a quasi-experimental study. BMC Med Ethics 2013;14:8. [Crossref] [PubMed]
- Center for Disease Control and Prevention. U.S. Department of Health and Human Services. 2022 [cited 2023 Apr 4]. Health Insurance Portability and Accountability Act of 1996 (HIPAA). Available online: https://www.cdc.gov/phlp/publications/topic/hipaa.html#:~:text=The%20Health%20Insurance%20Portability%20and,the%20patient’s%20consent%20or%20knowledge
- Gandhi TK. Now Is the Time to Routinely Ask Patients About Safety. Jt Comm J Qual Patient Saf 2023;49:235-6. [Crossref] [PubMed]
- Lu L, Ko YM, Chen HY, et al. Patient Safety and Staff Well-Being: Organizational Culture as a Resource. Int J Environ Res Public Health 2022;19:3722. [Crossref] [PubMed]
- Scott G, Hogden A, Taylor R, et al. Exploring the impact of employee engagement and patient safety. Int J Qual Health Care 2022;34:mzac059. [Crossref] [PubMed]
- Kożusznik MW, Peiró JM, Soriano A, et al. “Out of Sight, Out of Mind?”: The Role of Physical Stressors, Cognitive Appraisal, and Positive Emotions in Employees’ Health. Environ Behav 2018;50:86-115. [Crossref]
- Ceravolo DJ, Schwartz DG, Foltz-Ramos KM, et al. Strengthening communication to overcome lateral violence. J Nurs Manag 2012;20:599-606. [Crossref] [PubMed]
- Real K, Bardach SH, Bardach DR. The Role of the Built Environment: How Decentralized Nurse Stations Shape Communication, Patient Care Processes, and Patient Outcomes. Health Commun 2017;32:1557-70. [Crossref] [PubMed]
- Gharaveis A, Hamilton DK, Pati D, et al. The Impact of Visibility on Teamwork, Collaborative Communication, and Security in Emergency Departments: An Exploratory Study. HERD 2018;11:37-49. [Crossref] [PubMed]
- Naccarella L, Raggatt M, Redley B. The Influence of Spatial Design on Team Communication in Hospital Emergency Departments. HERD 2019;12:100-15. [Crossref] [PubMed]
- Zadeh RS, Shepley MM, Waggener LT. Rethinking efficiency in acute care nursing units: analyzing nursing unit layouts for improved spatial flow. HERD 2012;6:39-65. [Crossref] [PubMed]
- Zborowsky T, Bunker-Hellmich L, Morelli A, et al. Centralized vs. decentralized nursing stations: Effects on nurses’ functional use of space and work environment. HERD 2010;3:19-42. [Crossref] [PubMed]
- Yi L, Seo HB. The effect of hospital unit layout on nurse walking behavior. HERD 2012;6:66-82. [Crossref] [PubMed]
- Shin D, Kang M. A study improving a nurse’s walking path and staff visibility in general hospital wards. Journal of the Architectural Institute of Korea Planning & Design 2016;32:41-50. [Crossref]
- Copeland D, Chambers M. Effects of unit design on acute care nurses’ walking distances, energy expenditure, and job satisfaction: A pre–post relocation study. HERD 2017;10:22-36. [Crossref] [PubMed]
- Lee E, Daugherty J, Selga J, et al. Enhancing Patients’ wayfinding and visitation experience improves quality of care. Journal of PeriAnesthesia Nursing 2020;35:250-4. [Crossref] [PubMed]
- Pati D, Harvey TE Jr, Willis DA, et al. Identifying elements of the health care environment that contribute to wayfinding. HERD 2015;8:44-67. [Crossref] [PubMed]
- Renninger N, Nastasi N, Bope A, et al. Indoor Dust as a Matrix for Surveillance of COVID-19. mSystems 2021;6:e01350-20. [Crossref] [PubMed]
- Otter JA, Yezli S, Salkeld JA, et al. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control 2013;41:S6-11. [Crossref] [PubMed]
- Moccia G, Motta O, Pironti C, et al. An alternative approach for the decontamination of hospital settings. J Infect Public Health 2020;13:2038-44. [Crossref] [PubMed]
- Chemaly RF, Simmons S, Dale C Jr, et al. The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment. Ther Adv Infect Dis 2014;2:79-90. [Crossref] [PubMed]
- Watson F, Wilks SA, Keevil CW, et al. Evaluating the environmental microbiota across four National Health Service hospitals within England. J Hosp Infect 2023;131:203-12. [Crossref] [PubMed]
- Durant DJ. Can patient-reported room cleanliness measures predict hospital-acquired C. difficile infection? A study of acute care facilities in New York state. Am J Infect Control 2021;49:452-7. [Crossref] [PubMed]
- Carling PC, Briggs JL, Perkins J, et al. Improved cleaning of patient rooms using a new targeting method. Clin Infect Dis 2006;42:385-8. [Crossref] [PubMed]
- Morris ME, Webster K, Jones C, et al. Interventions to reduce falls in hospitals: a systematic review and meta-analysis. Age Ageing 2022;51:afac077. [Crossref] [PubMed]
- Pati D, Harvey TE, Reyers E, et al. A multidimensional framework for assessing patient room configurations. HERD 2009;2:88-111. [Crossref] [PubMed]
- Pati D, Lee J, Mihandoust S, et al. Top Five Physical Design Factors Contributing to Fall Initiation. HERD 2018;11:50-64. [Crossref] [PubMed]
- Lavender SA, Sommerich CM, Patterson ES, et al. Hospital Patient Room Design: The Issues Facing 23 Occupational Groups Who Work in Medical/Surgical Patient Rooms. HERD 2015;8:98-114. [Crossref] [PubMed]
- Kim D, Portillo M. Fall Hazards Within Senior Independent Living: A Case-Control Study. HERD 2018;11:65-81. [Crossref] [PubMed]
- Brewer BB, Carley KM, Benham-Hutchins M, et al. Nursing Unit Design, Nursing Staff Communication Networks, and Patient Falls: Are They Related? HERD 2018;11:82-94. [Crossref] [PubMed]
- Pati D, Pati S, Harvey TE Jr. Security Implications of Physical Design Attributes in the Emergency Department. HERD 2016;9:50-63. [Crossref] [PubMed]
- Knowles E, Mason SM, Moriarty F. ‘I’m going to learn how to run quick’: exploring violence directed towards staff in the Emergency Department. Emergency Medicine Journal 2013;30:926-31. [Crossref] [PubMed]
- Connellan K, Gaardboe M, Riggs D, et al. Stressed spaces: mental health and architecture. HERD 2013;6:127-68. [Crossref] [PubMed]
- Brophy JT, Keith MM, Hurley M. Assaulted and Unheard: Violence Against Healthcare Staff. New Solut 2018;27:581-606. [Crossref] [PubMed]
- Lenaghan PA, Cirrincione NM, Henrich S. Preventing Emergency Department Violence through Design. J Emerg Nurs 2018;44:7-12. [Crossref] [PubMed]
- Pati D, Gaines K, Valipoor S. Delivering Rural Health in a Changing Health Model: A Qualitative Study Involving Four Hospitals. HERD 2016;10:76-86. [Crossref] [PubMed]
- Person J, Spiva L, Hart P. The culture of an emergency department: an ethnographic study. Int Emerg Nurs 2013;21:222-7. [Crossref] [PubMed]
- Fay L, Cai H, Real K. A Systematic Literature Review of Empirical Studies on Decentralized Nursing Stations. HERD 2019;12:44-68. [Crossref] [PubMed]
- Hadi K, Zimring C. Design to Improve Visibility: Impact of Corridor Width and Unit Shape. HERD 2016;9:35-49. [Crossref] [PubMed]
- Lee Y. Workplace health and its impact on human capital: seven key performance indicators of workplace health. In: Korhan O, editor. Indoor environment and health. IntechOpen 2019.
- Mokarami H, Eskandari S, Cousins R, et al. Development and validation of a Nurse Station Ergonomics Assessment (NSEA) tool. BMC Nurs 2021;20:83. [Crossref] [PubMed]
- Galinsky T, Deter L, Krieg E, et al. Safe patient handling and mobility (SPHM) for increasingly bariatric patient populations: Factors related to caregivers’ self-reported pain and injury. Appl Ergon 2021;91:103300. [Crossref] [PubMed]
- Ramli AH. Work environment, job satisfaction and employee performance in health services. Business and Entrepreneurial Review 2019;19:29-42. [Crossref]
- Asuquo EG, Tighe SM, Bradshaw C. Interventions to reduce work-related musculoskeletal disorders among healthcare staff in nursing homes; An integrative literature review. Int J Nurs Stud Adv 2021;3:100033. [Crossref]
- Soylar P, Ozer A. Evaluation of the prevalence of musculoskeletal disorders in nurses: a systematic review. Med Sci 2018;7:479-85. [Crossref]
- Fujishiro K, Weaver JL, Heaney CA, et al. The effect of ergonomic interventions in healthcare facilities on musculoskeletal disorders. Am J Ind Med 2005;48:338-47. [Crossref] [PubMed]
- Ulrich RS, Berry LL, Quan X, et al. A conceptual framework for the domain of evidence-based design. HERD 2010;4:95-114. [Crossref] [PubMed]
- Ulrich RS. Effects of interior design on wellness: theory and recent scientific research. J Health Care Inter Des 1991;3:97-109. [PubMed]
- Kim YK, Kim SM, Myoung H. Musical intervention reduces patients' anxiety in surgical extraction of an impacted mandibular third molar. J Oral Maxillofac Surg 2011;69:1036-45. [Crossref] [PubMed]
- Beukeboom CJ, Langeveld D, Tanja-Dijkstra K. Stress-reducing effects of real and artificial nature in a hospital waiting room. J Altern Complement Med 2012;18:329-33. [Crossref] [PubMed]
- Vetter D, Barth J, Uyulmaz S, et al. Effects of Art on Surgical Patients: A Systematic Review and Meta-analysis. Ann Surg 2015;262:704-13. [Crossref] [PubMed]
- Ulrich RS, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. HERD 2008;1:61-125. [Crossref] [PubMed]
- Huisman ERCM, Morales E, van Hoof J, et al. Healing environment: A review of the impact of physical environmental factors on users. Build Environ 2012;58:70-80. [Crossref]
- Bakker AB, Demerouti E, Sanz-Vergel A. Job demands–resources theory: Ten years later. Annual Review of Organizational Psychology and Organizational Behavior 2023;10:25-53. [Crossref]
- Navajas-Romero V, Ariza-Montes A, Hernández-Perlines F. Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context. Int J Environ Res Public Health 2020;17:2847. [Crossref] [PubMed]
- Duane JN, Blanch-Hartigan D, Sanders JJ, et al. Environmental Considerations for Effective Telehealth Encounters: A Narrative Review and Implications for Best Practice. Telemed J E Health 2022;28:309-16. [Crossref] [PubMed]
- Pilosof NP, Barrett M, Oborn E, et al. Telemedicine Implementation in COVID-19 ICU: Balancing Physical and Virtual Forms of Visibility. HERD 2021;14:34-48. [Crossref] [PubMed]
- O'Brien M, McNicholas F. The use of telepsychiatry during COVID-19 and beyond. Ir J Psychol Med 2020;37:250-5. [Crossref] [PubMed]
- Lee J, Lee H, Shepley MM. Exploring the spatial arrangement of patient rooms for minimum nurse travel in hospital nursing units in Korea. Frontiers of Architectural Research 2020;9:711-25. [Crossref]
- Mitchell BG, Hall L, White N, et al. An environmental cleaning bundle and health-care-associated infections in hospitals (REACH): a multicentre, randomised trial. Lancet Infect Dis 2019;19:410-8. [Crossref] [PubMed]
- Rashid T, Vonville H, Hasan I, et al. Mechanisms for floor surfaces or environmental ground contamination to cause human infection: a systematic review. Epidemiol Infect 2017;145:347-57. [Crossref] [PubMed]
- Tse T. The environment and falls prevention: Do environmental modifications make a difference? Aust Occup Ther J 2005;52:271-81. [Crossref]
- Drahota A, Felix LM, Raftery J, et al. Shock-absorbing flooring for fall-related injury prevention in older adults and staff in hospitals and care homes: the SAFEST systematic review. Health Technol Assess 2022;26:1-196. [Crossref] [PubMed]
- Pati D, Valipoor S, Lorusso L, et al. The Impact of the Built Environment on Patient Falls in Hospital Rooms: An Integrative Review. J Patient Saf 2021;17:273-81. [Crossref] [PubMed]
- Zadeh RS, Shepley MM, Owora AH, et al. The importance of specific workplace environment characteristics for maximum health and performance: healthcare workers’ perspective. J Occup Environ Med 2018;60:e245-52. [Crossref] [PubMed]
- Bubric K, Harvey G, Pitamber T. A User-Centered Approach to Evaluating Wayfinding Systems in Healthcare. HERD 2021;14:19-30. [Crossref] [PubMed]
Cite this article as: Zamani Z, Joy T, Abbey M. Exploring environmental design attributes impacting staff perceptions of safety in a complex hospital system: implications for healthcare design. J Hosp Manag Health Policy 2023;7:21.

