Clinical practice review on population health management and promoting positive health outcomes
IntroductionOther Section
Population health management has gained worldwide momentum due to the pandemic of chronic conditions and comorbidities in diverse populations (1). According to the Centers for Disease Control and Prevention (CDC), chronic diseases are broadly defined as existing conditions lasting more than a year and require ongoing medical attention, such as heart disease, cancer, and diabetes (2). Population health management has been identified as a sustainable solution for integrated healthcare management that promotes patient/client outcomes for people diagnosed with chronic diseases (3). It is regarded as an essential health infrastructure dependent on collaborative data, interprofessional co-production and diverse knowledge and skills to manage patient’s/clients with long-term illnesses (4). Population health management are integrative and collaborative initiatives, that have emerged to close the gap between health and community services (5), with the intention of improving population health in communities and neighborhoods that may be disadvantaged or marginalized (6). With the growing number of population groups diagnosed with chronic diseases, avoidable health and social inequalities persist, resulting in debilitating effects on well-being, life expectancy and quality of life (7).
Chronic disease prevention is recognized as a beneficial management strategy for community-based and health systems sectors as it fosters linkages between healthcare, community and social services (8). Struijs et al. (1) believe that combining population health needs assessments with effective models of care and a collaborative interprofessional approach is necessary to promote health outcomes. This clinical practice review aimed to outline the key successes of population health management that promote positive health outcomes for people diagnosed with a chronic disease. The RIGHT checklist was used to guide the reporting process of this clinical practice review (9). It provided a systematic structure to ensure key components of the checklist were incorporated as part of the reporting process.
MethodsOther Section
We gathered evidence-based opinions and perspectives from published literature that had explored population health management for promoting positive health outcomes for people diagnosed with a chronic disease. We also included evidence-based perspectives from published literature including countries that utilized the population health management approach as a collaborative interprofessional management strategy. This clinical practice review was guided by the following questions: how effective is population health management? Does it promote positive health outcomes for patients/clients diagnosed with a chronic disease?
Search strategy
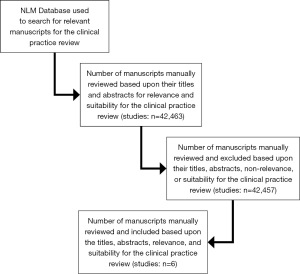
This clinical practice review was constructed using the National Library of Medicine (NLM) database. The search was targeted at an interprofessional approach to population health management, and the following search terms population, health, management, and outcomes were inserted into the database combined with Boolean search operators ‘AND’ and ‘OR’. We searched for manuscripts dated within the last 12 months to examine the most current opinions and perspectives on population health management and promoting positive health outcomes. The abstracts and titles were screened for relevance and appropriateness of this clinical practice review. Although there were an extensive number of manuscripts that appeared from the search, and despite the use of key words and Boolean operators, the authors continued to manually review abstracts and titles, accordingly, to ensure the inclusion of manuscripts that had a focus on the topic and questions being explored. It was evident through the review of the titles and abstracts which manuscripts were suited for this clinical practice review. An extensive review of the selected manuscripts was further conducted to ensure each of the selected manuscripts met the objectives of the clinical practice review. Table 1 was developed to facilitate the review of the selected manuscripts and to evaluate each publication for its outcome data. The criteria used for reviewing each of the selected manuscripts were the study outcomes and the strengths and limitations of population health management identified in each of the reviewed studies.
Table 1
| Author/year study published/reference | Country | Manuscript method | Outcome | Strengths and limitations of PHM |
|---|---|---|---|---|
| Abraham et al. Global Trends Towards Population Health Management and Key Lessons and Initiatives in the Singapore Context. Int J Integr Care 2022;22:19. (10) | Singapore | Editorial | To maximise population-wide health outcomes, decisions must be made around expanding the reach of population health interventions | Strengths: the recognition of the importance of data and information technology integration enables PHM |
| Limitations: further work is needed at the system-level to accelerate the impact of population health interventions | ||||
| Cianciara et al. Participation in Population Health Interventions by Older Adults in Poland: Barriers and Enablers. Int J Environ Res Public Health 2023;20:2284. (11) | Poland | Survey | Implementing interventions for older adults helps improve health outcomes and reduces social health inequities | Strengths: participation in population health interventions are enablers to successful outcomes |
| Limitations: older adults with a low level of education, seldom visits to their general practitioner and low social activity are barriers for population health interventions and positive outcomes | ||||
| ElSayed et al. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2023. Diabetes Care 2023;46:S10-8. (12) | USA | Standards of care | Health inequities related to diabetes and its complications are well documented, are heavily influenced by social determinants of health | Strengths: standardized sociodemographic variables in electronic health records facilitate the measurement of health inequities and the impact of interventions designed to reduce those inequities |
| Limitations: there is currently a paucity of evidence regarding enhancing resources that will benefit intervention strategies | ||||
| Mungmode et al. Making Diabetes Electronic Medical Record Data Actionable: Promoting Benchmarking and Population Health Improvement Using the T1D Exchange Quality Improvement Portal. Clin Diabetes 2022;41:45-55. (13) | USA | Standards of care | Understanding the quality of clinical care processes and services is essential to health care quality improvement | Strengths: population health summaries and outcome trends are a valuable tool for quality improvement |
| Limitations: mapping, validating, and transferring of data can be an obstacle if not regarded as a priority | ||||
| Pacileo et al. DM management in HIV patients: the adoption of population health management to transform the chronic management of HIV. Eur J Public Health 2022;32:942-7. (14) | Italy | Retrospective observational study | PHM approach represents a powerful tool for evaluating system capacity to manage HIV comorbidities | Strengths: the PHM approach understands the comorbidity burden in HIV patient management |
| Limitations: different solutions tailored to different contexts of HIV services will likely be required | ||||
| Steenkamer et al. Population health management in Belgium: a call-to-action and case study. BMC Health Serv Res 2023;23:659. (15) | Belgium | Virtual focus group | There is a need to instill a sense of urgency among all stakeholders to develop a joint population-oriented vision | Strengths: collaborative ownership and responsibility are needed from all stakeholder groups, as progress in PHM |
| Limitations: initiating new payment models for PHM may be a concern for stakeholders |
PHM, population health management; HIV, human immunodeficiency virus.
Eligibility criteria
Manuscripts were included if they were peer-reviewed with full-text access, related to population health management and advocated for integrative and collaborative initiatives that promote positive health outcomes as defined by Steenkamer et al. (5). The manuscripts that did not directly relate to population health management and promoting positive health outcomes for people diagnosed with a chronic disease were excluded. The decision-making process for selecting appropriate manuscripts for this clinical practice review, was determined by revisiting the titles and abstracts of the selected studies and publications to ensure that each of them was selected according to the clinical practice review objectives. It was essential that there was an agreed census among the authors regarding the appropriateness of each manuscript prior to them being included in the clinical practice review. It was also important that the selected manuscripts were relevant to help answer the questions that guided the clinical practice review.
ResultsOther Section
Characteristics of included studies
The number of manuscripts retrieved was limited due to the publication date and the specifics of the topic being reviewed. A total of six manuscripts in full text were accessed from the NLM database. The six papers were selected as they were relevant to the topic being explored, the key search criteria and provided data for this clinical practice review. The process of retrieving the manuscripts and selecting the articles included in this clinical practice review has been illustrated in a flow diagram (Figure 1) which complied with the RIGHT checklist for reporting a clinical practice review. Of the six manuscripts included in this review, two were papers on standards of care (12,13), one was an editorial (10), there was also a survey (11), a focus group study (15) and a retrospective observation (14).
The authors that focused on the standards of care had evaluated the effectiveness of implementation practices in population health management for promoting positive health outcomes for patient’s/clients diagnosed with a chronic disease. The editorial and focus group study discussed the global move towards population health management. The survey explored the enablers and barriers to participation in health programmes that promote positive health outcomes and the retrospective observation focused on population health management as a tool for evaluating care interventions. The findings from these studies and reports demonstrated the importance of various approaches to promoting health outcomes, strategic health management and implementing a collaborative approach to advance population health management.
DiscussionOther Section
The effectiveness of population health management
Cianciara et al. (11) have provided evidence that population health management is essential for promoting health outcomes for those living with and diagnosed with a chronic disease. Health technologies, teleconsultations and healthcare management without patient’s/clients needing to visit service providers have accommodated individuals within population health management (16). Telehealth, integration of data and the encouragement of patient/client involvement are aspects of population health management that have been essential for its effectiveness as a management strategy (17). Somani et al. (16) lay emphasis the impact of virtual services being the optimal method of minimizing service disruption when managing population groups, and Bakhit et al. has shown that digital health does not differ from in-person consultations and is an effective method of distanced management of chronic diseases (18). ElSayed et al. (12) believe that standardizing sociodemographic variables in electronic health records facilitates the measurement of health inequities and the impact of interventions designed to reduce health inequities within population groups. Although population health management has evolved globally, Steenkamer et al. believe there is a need to instill a sense of urgency among all stakeholders to develop a joint population-oriented vision. The lack of joint vision poses the risk of inadequate infrastructural building blocks that must be implemented to secure resources, technologies, finance and adequate leadership (19).
Population health management and improving health outcomes
Pacileo et al. (14) recognize that the population health management approach to care processes is a powerful tool for evaluating health outcomes for patient’s/clients diagnosed with human immunodeficiency virus (HIV) and other comorbidities. Integrative health care, using telehealth for disease management, and continuing care management is fundamental for improving health outcomes (20). According to Abraham et al. (10) maximizing population-wide health outcomes depends upon decisions that expand the reach of population health interventions across communities and those living with chronic diseases. It has been identified that population health management strategies achieve their aims by including co-production, strengthening the integration of primary care services, and targeting programmes that maximize health outcomes through strategic monitoring (21).
Mungmode et al. (13) emphasized the importance of population health management and outcome trends being a valuable tool for quality improvement, and incorporating it as a health management strategy for managing chronic diseases, especially for improving health outcomes for a population group with a debilitating condition (22). Evidence-based recommendations highlight the importance of patient/client assessment, level of engagement and evaluation of patient/client outcomes using telehealth methods (23). The reliance on individualized and non-collaborative care management for chronic diseases has become past practice. Cianciara et al. (11) highlight that implementing interventions to improve health outcomes helps reduce social health inequities and enable successful outcomes. Steenkamer et al. (15) believe collaborative ownership and responsibility are needed to progress population health management outcomes. However, it is also perceived to maximize collaborative healthcare delivery without compromising quality healthcare and safety (16).
With an ageing population and various chronic co-morbidities, improving and promoting positive health outcomes is essential for healthy population groups. The available data on advancing population health management and promoting positive health outcomes has shown a need for shared clinical and healthcare knowledge. The acceptance from stakeholders, patients/clients and the need for resources and digital infrastructure are fundamental. The future of population health management is optimistic, as integrative and collaborative healthcare management is essential for promoting positive health outcomes.
Implications for practice
Healthcare service providers should continue developing an integrative and collaborative approach to population health management to promote positive health outcomes. Cianciara et al. (11) has provided evidence on the importance of patient/client engagement with population health management programs, which has been welcomed by various populations diagnosed with chronic illnesses (24). Evidence shows that telehealth has successfully managed population groups in diverse community settings (16). Healthcare professionals could promote awareness of population health management by delivering educational seminars from an interprofessional approach focusing on the benefits of managing chronic disease through collaboration, intervention and promoting positive health outcomes. Regional funded educational programs that support population health management, are also initiatives that would help overcome health disparities and help to promote positive health outcomes for identified population groups who are living with various diagnosed chronic conditions.
Limitations
The number of manuscripts retrieved and included within this clinical practice review could have been improved. The included sources were limited due to the publication date and the scope of practice being explored. Thus, this may not give a comprehensive insight into population health management and promoting positive health outcomes. However, the reviewed manuscripts have highlighted the significance of collaborative and integrative care for those diagnosed with a chronic disease.
ConclusionsOther Section
The available literature on population health management and promoting positive health outcomes have demonstrated a sustainable and strategic method for managing a population group with a chronic disease. Undoubtedly, there is a need to monitor and evaluate the effectiveness of population health management. Healthcare professionals, stakeholders and healthcare service providers must work cohesively to maximize patient/client outcomes now and in the future.
AcknowledgmentsOther Section
The authors would like to thank Dr. Jacqueline Guendouzi, Professor, Department of Health and Human Sciences, Southeastern Louisiana University, for granting assigned time to conduct this clinical practice review.
Funding: None.
FootnoteOther Section
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-106/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-106/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Struijs JN, Drewes HW, Heijink R, et al. How to evaluate population management? Transforming the Care Continuum Alliance population health guide toward a broadly applicable analytical framework. Health Policy 2015;119:522-9. [Crossref] [PubMed]
- CDC. About Chronic Diseases. 2022. Available online: https://www.cdc.gov/chronicdisease/about/index.htm
- Lyles LF, Hildebrandt H, Mair A. Population Health Management Approach: Integration of Community-Based Pharmacists into Integrated Care Systems: Reflections from the U.S., Achievements in Scotland and Discussions in Germany. Int J Integr Care 2020;20:13. [Crossref] [PubMed]
- Cronin CE, Franz B, Schuller KA. Expanding the Population Health Workforce: Strategic Priorities of Hospital Organizations in the United States. Popul Health Manag 2021;24:59-68. [Crossref] [PubMed]
- Steenkamer BM, Drewes HW, Heijink R, et al. Defining Population Health Management: A Scoping Review of the Literature. Popul Health Manag 2017;20:74-85. [Crossref] [PubMed]
- Alderwick H, Ham C, Buck D. Population health systems: going beyond integrated care. 2015.
- Romero D, Echeverria SE, Duffy M, et al. Development of a wellness trust to improve population health: Case-study of a United States urban center. Prev Med Rep 2018;10:292-8. [Crossref] [PubMed]
- Lang A, Warren M, Kaulman L. A funding crisis for public health and safety: state-by-state public health funding and key health facts: 2018. Washington, DC, USA: Trust for America’s Health; 2018.
- Chen Y, Yang K, Marušic A, et al. A Reporting Tool for Practice Guidelines in Health Care: The RIGHT Statement. Ann Intern Med 2017;166:128-32. [Crossref] [PubMed]
- Abraham M, Lim MJ, Tan WS, et al. Global Trends Towards Population Health Management and Key Lessons and Initiatives in the Singapore Context. Int J Integr Care 2022;22:19. [Crossref] [PubMed]
- Cianciara D, Lewtak K, Poznańska A, et al. Participation in Population Health Interventions by Older Adults in Poland: Barriers and Enablers. Int J Environ Res Public Health 2023;20:2284. [Crossref] [PubMed]
- ElSayed NA, Aleppo G, Aroda VR, et al. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes-2023. Diabetes Care 2023;46:S10-8. [Crossref] [PubMed]
- Mungmode A, Noor N, Weinstock RS, et al. Making Diabetes Electronic Medical Record Data Actionable: Promoting Benchmarking and Population Health Improvement Using the T1D Exchange Quality Improvement Portal. Clin Diabetes 2022;41:45-55. [Crossref] [PubMed]
- Pacileo G, Morando V, Banks H, et al. DM management in HIV patients: the adoption of population health management to transform the chronic management of HIV. Eur J Public Health 2022;32:942-7. [Crossref] [PubMed]
- Steenkamer B, Vaes B, Rietzschel E, et al. Population health management in Belgium: a call-to-action and case study. BMC Health Serv Res 2023;23:659. [Crossref] [PubMed]
- Somani BK, Pietropaolo A, Coulter P, et al. Delivery of urological services (telemedicine and urgent surgery) during COVID-19 lockdown: experience and lessons learnt from a university hospital in United Kingdom. Scott Med J 2020;65:109-11. [Crossref] [PubMed]
- López-Fando L, Bueno P, Carracedo D, et al. Management of Female and Functional Urology Patients During the COVID Pandemic. Eur Urol Focus 2020;6:1049-57. [Crossref] [PubMed]
- Bakhit M, Baillie E, Krzyzaniak N, et al. Antibiotic prescribing for acute infections in synchronous telehealth consultations: a systematic review and meta-analysis. BJGP Open 2021;5:BJGPO.2021.0106.
- Steenkamer BM. Population Health Management unravelled: insights into transformations towards sustainable health and wellbeing systems. Tilburg University 2020.
- Medina-Polo J, Téigell Tobar J, Romero-Otero J, et al. Benign prostatic hyperplasia management during COVID-19 pandemia. Arch Esp Urol 2020;73:405-12. [PubMed]
- Pierce-Wrobel C, Miklos J. How The Most Successful ACOs Act As Factories Of Innovation. Health Affairs Blog 2018.
- Grimes CL, Balk EM, Crisp CC, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: review of existing evidence. Int Urogynecol J 2020;31:1063-89. [Crossref] [PubMed]
- Sacco E, Gandi C, Li Marzi V, et al. Extensive impact of COVID-19 pandemic on pelvic floor dysfunctions care: A nationwide interdisciplinary survey. Neurourol Urodyn 2021;40:695-704. [Crossref] [PubMed]
- Novara G, Checcucci E, Crestani A, et al. Telehealth in Urology: A Systematic Review of the Literature. How Much Can Telemedicine Be Useful During and After the COVID-19 Pandemic? Eur Urol 2020;78:786-811. [Crossref] [PubMed]
Cite this article as: Collins L, Ross L, Ugiagbe M. Clinical practice review on population health management and promoting positive health outcomes. J Hosp Manag Health Policy 2023;7:23.