Impact of COVID-19 on operation room utilization efficiency and cardiac surgery care pathway: single centre experience
Highlight box
Key findings
• Both surgical and anaesthetic efficiency suffered during the pandemic due to additional impositions in the cardiac surgery care pathway.
• Multiple variables contributing to COVID related delays include prolonged intensive care unit (ICU) stays, reduced surgical efficiency, and unexpected need for resource reprioritisation.
What is known and what is new?
• What is known is the significant diversion and reprioritisation of resources and human capital to COVID intensive areas, resulting in reduced cardiac surgery activity.
• Heightened focus on re-addressing the reprioritisation of resources early for COVID cases to repent late unexpected divergents and delays service provision.
What is the implication, and what should change now?
• Horizon scanning of admitted cases in acute medical wards may help re-prioritization of resources early.
• Delayed transfers to high-dependency units or the wards secondary to bed pressures resulted in delayed ICU discharges, and therefore prolonged ICU times. Prioritising resources and team efforts to maximise discharge efficiency from the wards during periods of increasing COVID numbers may help alleviate bed pressure and reduce unnecessary ICU stays.
• Unexpected outbreaks of COVID in the wards and mandatory isolation of contact patients contributed to lower operation room (OR) utilisation efficiency. Enforcing a stringent inpatient COVID screening program may detect COVID infections early and avoid spread, therefore optimising OR utilisation efficiency during COVID outbreaks.
Introduction
Novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (COVID-19) is a highly infectious RNA virus that spreads through respiratory droplets and has been associated with a global pandemic of unparalleled scale and suffering in modern times.
During the COVID-19 pandemic, the scale and rapidity of spread across the globe has caused an unprecedented and challenging impact on delivery of medical services. There has been wilful neglect of scientific advice early on in the pandemic (1,2). There was also political apathy and misguided national strategies during later stages that helped the unhindered propagation of the virus and numerous avoidable deaths (3-5). The virus continues to mutate genetically with emergence of new regional variants with greater infectivity but lower virulence. It is a hope that the impact of these newer strains on healthcare services would be less devastating.
Globally, national health services have been overwhelmed and there was drastic scaling down of specialist services. National emergency plans have been established to ring fence respiratory services, intensive care unit (ICU) beds and ventilator capacities and personnel have been redeployed to frontline areas with significant disruption of normal rotas and work shift patterns to aid in mitigation of human suffering and death toll of the pandemic. This has diverted resources and personnel from cardiac surgery services with severe curtailment of delivery of cardiac care (6-9). Despite the widespread impact, there have been no systematic reports or objective evaluation of the scale and scope of these changes in cardiac surgery and specially operation room (OR) utilization which is critical to the cardiac surgery care pathways (8-12).
The aim of this study was to assess OR utilization and efficiency in the COVID-19 lockdown period and compare it with the immediate preCOVID period in a quaternary multi-speciality teaching hospital in Southeast England. A secondary aim was to identify factors impacting OR utilization and efficiencies and the cardiac care pathway. The objective of this service improvement study was to use this analysis for recovery in the post lock down period and assimilate the experience gained and lessons learned for guidance during possible anticipated further waves of the pandemic. We present this article in accordance with the STROBE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-30/rc).
Methods
This retrospective single centre study was conducted as per the STROBE guidelines. We collected OR utilization data for the preCOVID period from 1st January 2020 to the day of the lockdown in England (23rd March 2020). All adult major cardiac cases were logged. This was compared to the OR data during the lockdown period up to 12th June 2020. The project was registered as a service improvement study (SafeGuard Audit 7151, SGH, 13/02/2022). All necessary approvals were obtained for use of data in compliance with local policies. Requirement for individual consent was waived due to the nature of the study (service improvement).
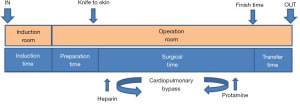
We used previously defined indices of OR utilization and efficiency to compare the data for the two periods (13). The operational pathway and definition of times are shown in Figure 1. Our calculations were based on a single 8 hour OR block with two cases on each OR list in the preCOVID period as the reference. The following calculations were used for OR efficiency (all times in minutes).
- Index of operational efficiency (InOE)
InOE (%) = 100 – [(total OR time − 240) × 100]/240 - Surgical efficiency (SE)
SE (%) = (surgical time/total OR time) × 100 - Anaesthetic efficiency (AE)
AE (%) = 100 – [(induction time + preparation time + sign out time)/total OR time] × 100 - Surgical index of operational efficiency (sInOE)
sInOE (%) = 100 – [(total OR time − surgical time) × 100]/240
Categorical variables were compared with Chi square test and continuous variables were compared with Man-Whitney U test. P value <0.05 was considered significant. All statistical analysis was done using SPSS v22.0 (IBM Corp, Armonk, NY, USA).
Figure 1 shows the new admission pathways that were implemented with COVID screening for urgent and emergency transfers and admissions. All elective surgery and training were stopped during the COVID period and all cases were done by consultants.
Results
Workflow and OR utilization
Total of 363 operations were logged during this period (preCOVID =304 and COVID period =59) (Table 1). There was a significant reduction in workflow for the period with overall 3 cases/day against an allocated OR capacity of 6 cases/day (for 3 ORs with average 2 blocks of 4 h/case). There was a significant reduction in cases/day (median 5 cases/day preCOVID to 1 case/day during COVID, P<0.001). OR utilization capacity was less than 50% for 36/65 (55.38%) COVID days vs. 5/59 (8.48%) preCOVID days (P<0.001). Almost half the COVID days (43.08%), there were no operations at all with completely wasted OR utilization vs. 0/59 (0%) preCOVID days.
Table 1
| Surgical variables | Overall (n=363) | PreCOVID (n=304) | COVID (n=59) | P value |
|---|---|---|---|---|
| Number of surgeries/day | 3 [1, 8] | 5 [1, 8] | 1 [1, 3] | <0.001 |
| Number of days with no operating (0 operations/day) | 28/124 (22.6) | 0/59 (0) | 28/65 (43.08) | <0.001 |
| Number of days with <50% operating (<3 operations/day) | 41/124 (33.07) | 5/59 (8.48) | 36/65 (55.38) | <0.001 |
| With CPB | 306/363 (84.3) | 260/304 (85.5) | 46/59 (77.9) | 0.19 |
| CABG | 118/363 (32.5) | 102/304 (33.6) | 16/59 (27.1) | 0.08 |
| Valves | 82/363 (22.6) | 70/304 (23.0) | 12/59 (20.3) | 0.08 |
| Others | 163/363 (44.9) | 132/304 (43.4) | 31/59 (52.5) | 0.09 |
| Without CPB | 5/363 (1.4) | 3/304 (0.99) | 2/59 (3.4) | 0.19 |
| Elective/urgent | 327/363 (90.1) | 275/304 (90.5) | 52/59 (88.1) | <0.001 |
| Median age, years | 68 [21, 87] | 69 [22, 87] | 62 [21, 84] | <0.001 |
| Log Euroscore | 5.1 [0.8, 64.53] | 4.7 [0.8, 64.53] | 6.6 [1.01, 54.55] | 0.193 |
| Bypass times | 107 [36, 410] | 107 [36, 410] | 111 [49, 308] | 0.66 |
| Cross clamp times | 77 [0, 278] | 77 [0, 278] | 76 [30, 248] | 0.85 |
Data are presented in median [IQR] or n/N (%). COVID, coronavirus disease; CPB, cardiopulmonary bypass; CABG, coronary artery bypass grafting; IQR, interquartile range.
Patient characteristics
Patients operated during COVID were younger (median 62 vs. 69 years, P<0.001) but higher risk (logistic Euroscore 6.6 vs. 4.7, P=0.193) (Table 1). There was no difference in bypass and cross clamp times. The cardiac intensive care units (CICU) stay was longer for COVID patients (51 vs. 48 h, P=0.05) although the intubation times and the overall length of stay did not change significantly. There was no reported mortality (urgent/elective cases) during the COVID period for the study vs. 1.09% preCOVID (P=0.004).
Times and operational efficiency indices
Induction times (56 min COVID vs. 49 min preCOVID, P=0.03) and sign out times (15 min COVID vs. 11 min preCOVID, P<0.001) were significantly longer for the COVID period (Table 2). Preparation times and surgical times were no different. The times and efficiency indices for coronary artery bypass grafting (CABG), valve and other procedures are shown in Figure 2 (also tabulated in Table 2). There was no difference in times and operational efficiencies for CABG. Induction times were significantly longer for COVID valve procedures (preCOVID 53 min vs. COVID 70 min, P<0.01). SE and AE were significantly reduced for COVID valve procedures (SE: preCOVID 75.4% vs. COVID 66%, P<0.01, AE: preCOVID 75.4% vs. COVID 66.6%, P<0.01). Similarly, SE and AE were significantly lower for ‘other’ procedures (SE: preCOVID 78.7% vs. COVID 71.9%, P<0.01, AE: preCOVID 76.1% vs. COVID 67.3%, P<0.01).
Table 2
| Operational variables | Overall (n=363) | PreCOVID (n=304) | COVID (n=59) | P value |
|---|---|---|---|---|
| Intraoperative | ||||
| Induction time (min) | 50 [0, 358] | 49 [0, 335] | 56 [0, 159] | 0.03 |
| Preparation time (min) | 10 [0, 359] | 11 [0, 75] | 10 [0.9, 69] | 0.09 |
| Surgical time (min) | 213 [9.9, 485] | 215 [9.9, 485] | 210 [15, 465] | 0.48 |
| Sign out time (min) | 12 [0, 358] | 11 [0, 135] | 15 [0, 40] | <0.001 |
| Total intraoperative time (min) | 295 [750, 625] | 294 [750, 625] | 295 [0, 570] | 0.834 |
| Efficiency indices | ||||
| InOE, % | 78 [−60, 737] | 78.8 [−60, 737] | 79 [−38.8, 93.6] | 0.90 |
| SE, % | 73.8 [−38, 357] | 74 [−25, 115] | 68.5 [−38.8, 93.6] | <0.001 |
| Anaesthetic efficiency (%) | 73.705 [1.3, 93] | 74.75 [1.3, 95.14] | 68.8 [19.79, 93.6] | <0.001 |
| sInOE, % | 31.25 [−543, 358] | 30 [−37, 147] | 35.4 [−543, 74.6] | 0.01 |
| Postoperative | ||||
| Intubation (h) | 15 [0, 432] | 15 [0, 432] | 15.5 [1, 324] | 0.391 |
| CICU stay (h) | 50 [1, 710] | 48 [1, 710] | 51 [16, 477] | 0.05 |
| Length of stay (days) | 12 [0, 328] | 11 [0, 126] | 16 [6, 63] | 0.32 |
| Inpatient mortality (elective/urgent?) | 3/327 (0.92) | 3/275 (1.09) | 0/52 | 0.004 |
| Inpatient mortality (emergency/salvage) | 6/36 (16.67) | 6/29 (20.69) | 0/7 | 0.629 |
Data are presented in median [IQR] or n/N (%). COVID, coronavirus disease; InOE, index of operational efficiency; SE, surgical efficiency; sInOE, index of surgical efficiency; CICU, cardiac intensive care unit; IQR, interquartile range.

Overall, surgical efficiency and anaesthetic efficiency suffered during the COVID pandemic (statistically significant changes were −7.4%, −5.0% respectively). InOE remained unchanged whereas sInOE improved 5.4%.
Length of ICU stay was significantly longer for COVID (preCOVID 48 h vs. COVID 51 h, P=0.05) although intubation times in ICU did not change significantly. There were no recorded inpatient cardiac mortalities during COVID period.
Discussion
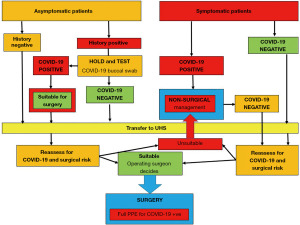
There has been a great reduction in the number of operated cardiac surgery cases worldwide during the pandemic (14-17). Utilization and efficiency in the cardiac OR remain central to resource and manpower consumption, revenues, and output through the overall cardiac surgery care pathway. COVID-19 pandemic created an unprecedented emergency with reduced efficiencies and loss of OR and ICU capacity. Several standard operational procedures (SOPs) were modified to screen patients and staff and reduce cross infections in critical areas such as OR and ICUs. This was a retrospective analysis at the height of the first wave of the COVID-19 pandemic in England. Previous UK reports have confirmed strategies and reduction in operative work during the pandemic but failed to objectively evaluate utilization and efficiencies in critical parts of the care pathway (18,19). The challenge has been to mitigate cross-infection and maintain efficient workflow in the critical parts of the cardiac surgery care pathway despite constrained resources and manpower (20-23). We concentrated on specific analysis of the OR part of the pathway to assess impact of COVID-19 on delivery of specialist cardiac services. There were changes for screening of patients for urgent and emergency surgeries during the pandemic. All elective surgery was completely stopped due to pressure on resources and manpower during various stages of the pandemic. A brief outline of the patient care pathway for admissions and acceptance for surgery is provided in Figure 3.
This analysis is the first of its kind to objectively analyse the workflow and efficiencies in the OR in a cardiac surgical care pathway. We further analysed the impact of other changes in the wider pathway on these measures. We evaluated both start time tardiness using knife to skin time and measures for middle and later parts of the operational pathway for anaesthetic induction times, preparation time, surgical times, and transfer times. Although the surgical, nursing, and anaesthetic teams work in synergy in the OR, the physical space, responsibilities, and the additional pressures imposed on each team are distinctly different. The induction room is a distinct space separate from the actual OR. We considered this as an extended OR for reasons of simplification of our analysis. We therefore evaluated surgical efficiency (essentially the surgical times) as separate from anaesthetic efficiency (essentially the induction, preparation, and transfer times) to gain greater insight into these team specific parts of the OR pathway. Both surgical and anaesthetic efficiency are specific case-based evaluation tools as opposed to InOE and sInOE which measure efficiencies over an entire OR utilization day (blocks of two 4 hr sessions each).
Safety of healthcare personnel was considered paramount, and steps were taken to reduce cross infections. Lateral flow tests and polymerase chain reaction (PCR) tests were mandatory for staff on a weekly basis. SOPs were modified for the induction room for aerosol generating procedures as per Department of Health guidance during the pandemic (24). These steps did not have a significant impact on induction times.
The database did not capture delays and cancellations due to redeployment and staff shortages (i.e., operating department/anaesthetic practitioners, operating room nurses). Although these could not be factored into the analysis, they were some of the most critical reasons for inefficiencies, case cancellations and wasted OR utilization. Staff shortages especially due to sick leave, mandatory isolation among contacts and those themselves testing COVID+ve remained a significant concern at the height of the pandemic. These shortages were also compounded by lockdowns, closure of schools and changing isolation rules imposing additional social pressures on carers and those with young families. Brexit and COVID related travel restrictions further made it difficult to recruit additional nursing and medical staff from the continent. A summary analysis of the additional pressures imposed on the distinct teams with COVID specific potential delays and inefficiencies is presented in Table 3.
Table 3
| Anaesthetic | Surgical | Nursing |
|---|---|---|
| Confirmation of COVID status | Previous case over run | Staff shortages (ICU nurses) |
| Delay in sending | All day complex case | Late admission/arrival |
| Staff shortages (ODP, AP) | Late first case start | Incomplete work up |
| Availability of blood | No suitable case identified | |
| Late ICU bed availability | Clinical cancellation (diarrhoea, fever, more investigations needed) | |
| Staff shortage (SCP, assistant, surgeon) |
COVID, coronavirus disease; ICU, intensive care unit; ODP, operating department practitioner; AP, anaesthetic practitioner; SCP, surgical care practitioner.
Operating with full class 4 personal protective equipment (PPE) was considered inconvenient by many staff. A particular problem was use of surgical loupes by surgeons with PPE. Tight fitting COVID masks were uncomfortable for long procedures without breaks for the surgical and nursing teams. Only two patients with indeterminate COVID status needed emergency operations in full PPE. Our analysis confirms that there were significant delays in induction time and sign out times as a result of these new measures although the surgical time and total operative time did not change significantly.
For individual cases, both the surgical and anaesthetic efficiency suffered during the pandemic due to additional impositions in the care pathway. Although these differences were statistically significant, practical time differences were small and probably inconsequential. The overall operative times did not differ significantly despite differences in some case types. Over the entire day, block operation efficiencies could be maintained. However, these overall block efficiencies need to be interpreted cautiously since there was significant OR under-utilization during COVID. Due to the case specific nature of our analysis, a number of reasons for delays, inefficiency and cancellations could not be captured (Table 3). Delay in sending, availability of blood, waiting for COVID test results for emergency patients, case overruns due to increased complexity of cases resulting in 2nd case cancellations were some of the most important reasons for inefficiency in the system. Late unforeseen cancellations due to COVID outbreaks in the ward and mandatory isolation of contact patients in the same bays and work areas was also an important unaccounted reason for lower OR utilization efficiency. The length of ICU was longer during COVID despite similar intubation times. Delayed transfers to high-dependency unit (HDU)/wards due to bed pressures and delayed discharges accounted for these prolonged ICU times.
Significant diversion and reprioritization of resources and human capital to COVID intensive areas (i.e., respiratory care wards and general ICU) caused a precipitous decline in overall cardiac activity. These reprioritization decisions were made at senior management levels to maintain overall workflow in the hospital due to splurge in COVID admissions and therefore remain justified. With emergence of lower virulence strains, and increasing vaccination coverage, such stringent reprioritizations may be less necessary in the future. Horizon scanning of admitted cases in acute medical wards may help re-prioritization. The pressure with these newer less virulent COVID strains may be more on HDU and ward beds rather than ICU beds due to infrequent demands for invasive ventilation in infected patients. Ring fencing of cardiac ICU beds to ensure some continuity of cardiac activity may be possible in the future outbreaks. Our analysis further confirms that despite the disruptions in the care pathway and effected changes, case operational efficiencies could be maintained at essentially preCOVID levels. Lessons can be learned from this analysis to identify areas of improvement and prioritization in anticipation of any further waves of new strains of COVID.
Limitations
This is a single centre retrospective analysis with small case numbers. Wasted efficiency due to time between cases was not factored into calculations for InoE and sInoE as this data was not available. Due to the case based nature of the analysis, some of the important reasons for delays and inefficiency in the overall care pathway could not be adequately captured.
Conclusions
COVID caused a significant disruption in patient care pathways in cardiac surgery. Operational service could be delivered to high efficiency despite significant changes. There was significantly decreased workflow due to reprioritization of resources.
Acknowledgments
We thank Mr. Bradley Yee, Senior Data Manager for help with the collection of data.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-30/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-30/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-30/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-30/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The project was registered as a service improvement study (SafeGuard Audit 7151, SGH, 13/02/2022). All necessary approvals were obtained for use of data in compliance with local policies. Requirement for individual consent was waived due to the nature of the study (service improvement).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamey G, Gonsalves G. Donald Trump: a political determinant of covid-19. BMJ 2020;369:m1643. [Crossref] [PubMed]
- Rinaldi C, Bekker MPM. A Scoping Review of Populist Radical Right Parties' Influence on Welfare Policy and its Implications for Population Health in Europe. Int J Health Policy Manag 2021;10:141-51. [PubMed]
- Abbasi K. COVID-19: Social murder, they wrote—elected, unaccountable, and unrepentant. BMJ 2021;372:n314. [Crossref] [PubMed]
- Worldometer. Reported cases and deaths by country or territory, accessed 10 Feb 2021. Available online: https://www.worldometers.info/coronavirus. Accessed - 12th Feb 2022
- Villani L, McKee M, Cascini F, et al. Comparison of Deaths Rates for COVID-19 across Europe During the First Wave of the COVID-19 Pandemic. Front Public Health 2020;8:620416. [Crossref] [PubMed]
- Patel S, Kaushik A, Sharma AK. Prioritizing cardiovascular surgical care in COVID-19 pandemic: Shall we operate or defer? J Card Surg 2020;35:2768-72. [Crossref] [PubMed]
- Dhingra NK, Verma S, Yau TM, et al. Stuck between a rock and a hard place: The clinical conundrum of managing cardiac surgical patients during the SARS-CoV-2 pandemic. J Card Surg 2022;37:174-5. [Crossref] [PubMed]
- Bashir M, Moughal S. Cardiovascular disease and surgery amid COVID-19 pandemic. J Vasc Surg 2020;72:405-7. [Crossref] [PubMed]
- Perek B, Olasinska-Wisniewska A, Misterski M, et al. How the COVID-19 pandemic changed treatment of severe aortic stenosis: a single cardiac center experience. J Thorac Dis 2021;13:906-17. [Crossref] [PubMed]
- Gopal K, Krishna N, Jose R, et al. Effects of the COVID-19 Pandemic on Cardiac Surgery Practice and Outcomes. J Chest Surg 2022;55:61-8. [Crossref] [PubMed]
- Greene A, Sapp J, Hirsch G, et al. Cardiovascular Outcomes in Nova Scotia During the Early Phase of the COVID-19 Pandemic. CJC Open 2022;4:324-36. [Crossref] [PubMed]
- Wang X, Gao H, Zhang Z, et al. Effect of the COVID-19 pandemic on complications and mortality of patients with cardiac surgery. J Cardiothorac Surg 2021;16:361. [Crossref] [PubMed]
- Luthra S, Ramady O, Monge M, et al. "Knife to skin" time is a poor marker of operating room utilization and efficiency in cardiac surgery. J Card Surg 2015;30:477-87. [Crossref] [PubMed]
- Bonalumi G, Giambuzzi I, Buratto B, et al. The day after tomorrow: cardiac surgery and coronavirus disease-2019. J Cardiovasc Med (Hagerstown) 2022;23:75-83. [Crossref] [PubMed]
- Wynne R, Smith JA. Cardiac Surgery in Australia During the COVID-19 Global Pandemic. Heart Lung Circ 2021;30:1800-4. [Crossref] [PubMed]
- Worthington T, Khoynezhad A. A Perspective from Los Angeles of COVID-19 effect and impact on cardiac surgery. J Card Surg 2021;36:1665-7. [Crossref] [PubMed]
- Farrington WJ, Mack CA, Karas MG, et al. A Perspective from New York of COVID 19: Effect and impact on cardiac surgery. J Card Surg 2021;36:1668-71. [Crossref] [PubMed]
- Harky A, Harrington D, Nawaytou O, et al. COVID-19 and cardiac surgery: A perspective from United Kingdom. J Card Surg 2021;36:1649-58. [Crossref] [PubMed]
- Lopez-Marco A, Harky A, Verdichizzo D, et al. Early experience of aortic surgery during the COVID-19 pandemic in the UK: A multicentre study. J Card Surg 2021;36:848-56. [Crossref] [PubMed]
- Engelman DT, Lother S, George I, et al. Adult cardiac surgery and the COVID-19 pandemic: Aggressive infection mitigation strategies are necessary in the operating room and surgical recovery. J Thorac Cardiovasc Surg 2020;160:447-51. [Crossref] [PubMed]
- Haft JW, Atluri P, Ailawadi G, et al. Adult cardiac surgery during the COVID-19 pandemic: A tiered patient triage guidance statement. J Thorac Cardiovasc Surg 2020;160:452-5. [Crossref] [PubMed]
- Luc JGY, Ad N, Nguyen TC, et al. Cardiac surgeons' concerns, perceptions, and responses during the COVID-19 pandemic. J Card Surg 2021;36:3040-51. [Crossref] [PubMed]
- Benedetto U, Goodwin A, Kendall S, et al. A nationwide survey of UK cardiac surgeons' view on clinical decision making during the coronavirus disease 2019 (COVID-19) pandemic. J Thorac Cardiovasc Surg 2020;160:968-73. [Crossref] [PubMed]
- Available online: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control. Accessed – 12th Feb 2022.
Cite this article as: Luthra S, Hunduma G, Navaratnarajah M, Malvindi PG, Goddard N, Miskolczi S, Velissaris T. Impact of COVID-19 on operation room utilization efficiency and cardiac surgery care pathway: single centre experience. J Hosp Manag Health Policy 2023;7:15.