
Effect of coronavirus disease 2019 (COVID-19) on orthopaedic surgical volume
Highlight box
Key findings
• Orthopaedic subspecialties like adult reconstruction, hand, spine, foot, and pediatrics had a large decrease in volume due to COVID-19 but recovered rapidly within months.
What is known and what is new?
• The COVID-19 pandemic has impacted healthcare delivery and orthopaedic surgical volume around the world.
• It is unclear how the COVID-19 pandemic differentially affected orthopaedic subspecialty surgical volume and how hospitals were able to recover.
What is the implication, and what should change now?
• Orthopaedic surgeons should be mindful of these trends prior to ratifying new agreements.
Introduction
Coronavirus disease 2019 (COVID-19) has had a significant impact on practice patterns for orthopedic surgeons across the globe. As of January 2023, in the United States the COVID-19 pandemic has resulted in over 1,500,000 deaths from 102 million reported cases (1). While many hospitals systems in the US have weathered multiple waves of cases, we have seen dramatic changes in the practice patterns of orthopedic services across the nation. Changes to orthopedic practice largely seem to be guided by the principles of clinical urgency, patient and healthcare worker protection, and conservation of health-care resources (2).
The global situation continues to evolve, and multiple organizations have offered guidance for the management of orthopaedic emergencies and resumption of elective orthopaedic cases (3-6). Consensus recommendations for limitation of non-urgent surgical procedures led to a halt on elective orthopaedic surgeries in a multitude of regions. A meta-analysis of 11 reviews from nine different health organizations demonstrated consensus guidance for either complete postponement of non-elective surgical procedures (63.6%), or selective postponement of these procedures (36.4%) (7). Consequently, a backlog of surgical cases and clinical visits is one of the most immediate challenges faced by healthcare organizations and their providers. The general guidance provided by consensus reports is to increase consideration for non-operative treatment options whenever possible and safe. As elective surgery begins to re-open, non-operative management will play a key role in managing the surgical backlog caused by the elective surgery shutdown (7). In addition, with the support of the Center for Medicare and Medicaid Service (CMS) and private insurance carriers, telemedicine initiatives have been quickly supported and enacted in order to continue providing health care to patients during the pandemic (8,9).
Among changes to elective orthopedic surgical volume, the volume of orthopaedic trauma surgeries performed at large trauma centers has also seen significant variance. The nature of this change is multifactorial and likely dependent on several characteristics that vary on a global, national, and regional scale. In the US, it’s likely that the influence of state and local governmental polices to isolate and quarantine, as well as social perception of health risks, have had an impactful role in reducing high injury-risk activity of a regional populace and driving reluctance to enter a hospital system unless necessary. Simply, even a reduction in motor vehicle travel could lead to reduced orthopedic trauma presenting to hospitals. There is evidence of these changes globally as well. University of Hong Kong Hospitals examined 928,278 patient-episodes, finding a reduction in orthopedic surgical volume of 44.2%. Elective joint replacement and ligament reconstruction decreased by between 74% and 84%, while upper and lower limb fracture treatment decreased by 23% and 20%, delineating a change in ratios of trauma to elective surgeries performed from 1.127:1 to 3.78:1 (10). In addition to epidemiological changes, early outcomes studies examining orthopaedic trauma patients have demonstrated change. In addition to direct effects of COVID pneumonia, changes to the delivery of orthopaedic services, particularly redistribution of human resources and disruption to continuity of care, have been implicated in increased 30-day mortality seen in femoral neck fractures and overall length of stay increases (11,12). Recent studies have alluded that older patients with medical comorbidities are more adversely affected by COVID-19 infections, owing to their diminished functional reserves and weakened immune systems (13-16). Therefore, it is critical that recommendations for practice management take the bimodal distribution and varied demographics of the orthopaedic trauma patient into account (3-6).
Despite unpredictable changes to practice volume, orthopaedic trauma and disease continue to occur and require treatment. As we move towards the resumption of the “new normal” standard of orthopedic practice in a post-pandemic world, it is imperative to understand current trends in surgical case load with the aim of predicting future changes. Our goal was to evaluate changes in orthopaedic subspecialty volume due to the COVID-19 pandemic in 2020 and compare these trends with orthopaedic subspecialty volume in 2019. We hypothesized a slow resurgence in orthopaedic volume at our center. We present this article in accordance with the STROBE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-16/rc).
Methods
The present study is an observational retrospective cohort study taking place at a large academic medical center. Data pertaining to operative volume was collected from the institution’s operating room ledger. Surgical volume between January 1 and August 31 was comparatively evaluated between 2019 (COVID-19-free) and 2020 (COVID-19). Initially total orthopaedic volume was assessed, then stratified by subspecialty including trauma, hand/sports/upper extremity, adult reconstruction, spine, foot and ankle, oncology, and pediatrics. Special care was taken to review all surgical procedures to ensure that all booked cases proceeded with surgery. At our institution, the first case of COVID-19 was recorded on March 12, 2020, and subsequently elective orthopaedic surgeries were paused between March 20, 2020, and May 11, 2020, as mandated by the state. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Albany Medical Center Institutional Review Board (IRB No. 00007321) and informed consent was taken from all the patients.
Study design
Orthopaedic procedures were stringently screened, and duplicate or cancelled procedures were removed prior to analysis. Next, all procedures were sorted by orthopaedic subspecialty based on the type of procedure and surgeon. Trauma included internal and external fixations, irrigation and debridement, and amputation procedures, among others. Upper extremity included hand (including trauma), shoulder, and sports medicine procedures that were not already included in the trauma cohort. Adult reconstruction included hip and knee arthroplasty, revision arthroplasty, and manipulations. Spine included debridement, discectomies, laminectomy, and decompression procedures. Foot and ankle included all foot or ankle procedures that were not trauma, including ankle replacement, ankle fusion, and metatarsal procedures. Oncology included tumor resections and biopsies. Pediatrics included all procedures performed on patients 18 years or younger.
Statistical analysis
Descriptive statistics were utilized to evaluate monthly orthopaedic surgical volume by subspecialty. Chi-square tests were performed to compare monthly orthopaedic surgical volume before the COVID-19 pandemic in 2019 and during the COVID-19 pandemic in 2020.
Results
In total, 8,170 orthopaedic procedures were completed at our medical center between January and August 2019 (n=4,243) and January and August 2020 (n=3,927). In March 2020, surgical volume decreased 28.7% compared to March 2019 following COVID-19 executive ordinances that paused all elective surgery at our institution on March 20, 2020. As COVID-19 cases in our region sharply increased in April 2020, orthopaedic surgical volume decreased 56.2% compared to April 2019 (Figure 1, Table 1). This large reduction in surgical volume was due to a severe decrease in adult reconstruction (−88.8%) and hand/upper extremity (−84.5%) volume, a moderate decrease in spine (−67.3%), foot (−58.1%), and pediatric (−49%) volume, and a slight change to trauma (−23.7%) and tumor (+33%) volume. The pause on elective surgeries at our institution was reversed on May 11, 2020, resulting in a month to month increase in overall surgical volume of 79.7% from April to May 2020. Between June and August 2020, average monthly orthopaedic surgical volume increased 15.2% compared to 2019. Altogether, the orthopaedic surgical volume between January and August 2020 decreased 7.4% compared to orthopaedic surgical volume between January and August 2019 and differed significantly (P<0.0001).
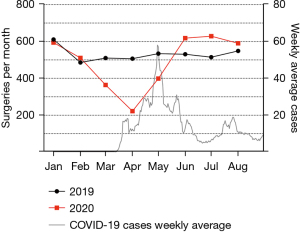
Table 1
| Month | Trauma | Adult reconstruction | Upper extremity | Spine | Foot | Pediatric | Tumor | Total |
|---|---|---|---|---|---|---|---|---|
| 2019 | ||||||||
| January | 207 | 168 | 64 | 62 | 49 | 36 | 25 | 611 |
| February | 163 | 128 | 63 | 35 | 33 | 40 | 24 | 486 |
| March | 162 | 126 | 63 | 51 | 47 | 40 | 21 | 510 |
| April | 156 | 125 | 71 | 52 | 43 | 45 | 15 | 507 |
| May | 155 | 144 | 69 | 63 | 44 | 41 | 18 | 534 |
| June | 175 | 137 | 59 | 47 | 37 | 58 | 18 | 531 |
| July | 186 | 125 | 49 | 53 | 48 | 39 | 15 | 515 |
| August | 204 | 126 | 63 | 45 | 30 | 58 | 23 | 549 |
| 2020 | ||||||||
| January | 196 | 163 | 82 | 50 | 45 | 42 | 16 | 594 |
| February | 163 | 145 | 65 | 45 | 29 | 47 | 17 | 511 |
| March | 131 | 90 | 49 | 32 | 22 | 30 | 10 | 364 |
| April | 119 | 14 | 11 | 17 | 18 | 23 | 20 | 222 |
| May | 136 | 89 | 45 | 36 | 28 | 46 | 19 | 399 |
| June | 195 | 151 | 76 | 61 | 50 | 56 | 29 | 618 |
| July | 239 | 141 | 70 | 56 | 51 | 55 | 17 | 629 |
| August | 235 | 148 | 51 | 46 | 30 | 57 | 23 | 590 |
| P value | 0.0063 | <0.0001 | <0.0001 | 0.0002 | 0.0057 | 0.0818 | 0.1714 | <0.0001 |
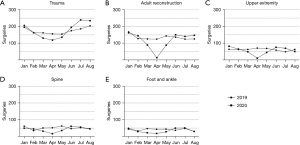
The COVID-19 pandemic affected the volume of orthopaedic subspecialties differently. Orthopaedic trauma, adult reconstruction, upper extremity, spine, and foot monthly surgical volume in 2020 differed significantly from 2019 (P=0.0063, P<0.0001, P<0.0001, P=0.0002, P=0.0057; Chi-square test). Trauma surgical volume experienced a monthly decrease of 18.4% between March and May 2020 during the pandemic-related local shutdowns compared to 2019 (Figure 2A, Table 1). Subsequently, average monthly trauma surgical volume increased 18.4% compared to 2019 volumes between June and August 2020. Adult reconstruction, upper extremity, spine, and foot experienced a substantial average decrease in monthly surgical volume of 51.1%, 48.3%, 48.8%, and 49.3% between March and May 2020 compared to 2019 volumes during the pause on elective procedures at our institution (Figure 2B-2E, Table 1). These subspecialties rapidly recovered leading to an average increase in average monthly surgical volume of 13.4%, 15.2%, 12.4%, and 13.9% between June and August 2020 compared to 2019 volumes.
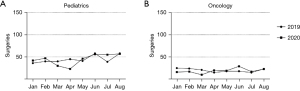
Pediatric orthopaedics and orthopaedic oncology monthly surgical volume in 2020 were not significantly different from corresponding monthly surgical volume in 2019 (P>0.05). Pediatric orthopaedic average monthly surgical volume decreased by 21.4% between March and May 2020 and increased by 8.4% between June and August 2020 compared to 2019 volumes (Figure 3A, Table 1). Orthopaedic oncology monthly surgical volume decreased an average 38.6% between January and March 2020 and increased an average 21.3% between April and August 2020 compared to 2019 (Figure 3B, Table 1). These changes in orthopaedic oncology volume did not correspond with the timing of the COVID-19 related restrictions in our region.
Discussion
The COVID-19 pandemic has led to significant guidelines and restrictions imposed on healthcare systems. These regulations continue to evolve based on new clinical data and epidemiological trends. With an emphasis on reallocation of essential staff and resources, government shutdowns on elective procedures resulted in impactful disruptions in hospital surgical volumes.
Our findings highlight the significant disruptions in case volumes observed by orthopaedic surgical subspecialties in a tertiary care center secondary to imposed COVID-19 restrictions. Following executive ordinances to pause all elective surgeries in March 2020, orthopedic surgical volume decreased 28.7% in March and 56.2% in April, compared to 2019 monthly volumes. Specific orthopaedic surgical subspecialties were impacted differently, with adult reconstruction (−88.8%) and hand/upper extremity (−84.5%) experiencing the most severe reductions in case volume. The trauma surgical volume (−23.7%) experienced a slight reduction in case volume, while orthopaedic tumor and pediatric orthopaedics saw an insignificant change in volume compared to 2019. Following reversal of the pause of elective surgeries in May 2020, our institution saw an immediate increase in overall orthopaedic surgical case volume (+79.7%) from April to May 2020. Surgical volume continued to increase in June and August compared to 2019. The strong rebound in case volumes served to hasten some of the effect of the pause on elective cases. Overall, between January and August 2020, monthly orthopaedic surgical volume significantly differed compared to 2019.
Although a robust recovery in surgical case volumes was observed at our institution, the magnitude of recovery differed by orthopaedic subspecialties. The orthopaedic trauma surgical volume initially experienced a minor decrease in volume, but swiftly recovered and even exceeded surgical volume from the previous year. As the largest tertiary center in the region, a portion of this increase in trauma volume was secondary to increased transfers from smaller regional hospital centers. In contrast, the adult-reconstruction, upper extremity, and spine subspecialties experienced a more severe reduction in volume. This highlights the economic perils that smaller regional hospital centers are facing due to COVID-19. Elective procedures account for 48% of hospital costs and potentially an even larger percentage of revenues (17). Five musculoskeletal procedures (hip arthroplasty, knee arthroplasty, laminectomy, spinal fusion, and treatment of lower extremity fracture or dislocation) account for 17% of all operating room procedures in US hospitals (17). A nationwide analysis of elective surgical case volume from academic and private hospitals across 21 US states observed a rapid decline in elective cases following the executive ordinance in March 2020, with as high as a 71% reduction in weekly case volume compared to 2019 (18). Consequently, while larger hospital systems may be able to weather the economic impact of the pandemic, the loss of revenue secondary to the pause on elective procedures may force many smaller hospital systems to shut down orthopaedic subspecialties and furlough employees. As a result, larger tertiary centers should prepare to see an increase in orthopaedic case volume, and we expect an increasing trend towards consolidation with larger, established hospital systems. These larger hospital systems will also be more desirable for newly trained hospital personnel as they can provide more financial security and stable income amid these uncertain times.
With an expected increase in orthopaedic case volume at large tertiary centers, orthopaedic surgeons should be mindful of overspecialization and limiting their scope of practice. Over 90% of graduating orthopaedic residents now pursue fellowship training, and only 15% of practicing orthopaedic surgeons now characterize themselves as generalists (19). Overspecialization exposes a surgeon’s practice to risk if demand or availability for a particular service disappears. This increasing trend towards sub-specialization may limit the clinical footprint of orthopaedic surgeons in the event of another pandemic or global crisis. It is ideal that orthopaedic surgeons possess a broad knowledge in the musculoskeletal field so that they can readily adapt to future unprecedented circumstances.
The COVID pandemic is unique in that it has also adversely affected orthopaedic resident training. The rapid migration of surgical case volumes to ambulatory surgical centers (ASCs) has caught many residency programs off guard as they may not have access to these sites. Complicating matters, many of these ASCs are frequently managed by for profit entities making it difficult to integrate meaningful surgical education. Additionally, social distancing regulations and reallocation of resources have led to drastic changes in resident didactics. Thanks to technological advances, some institutions have supplemented their resident education with simulation-based training and augmented reality (20,21). Although these novel learning approaches serve a valuable role, it is uncertain how effective they will be in providing residents with the necessary technical and non-technical surgical skills amid decreased surgical volume (20). Orthopaedic practices should be cognizant of the significant impact the pandemic has had on surgical training when hiring recent graduates. Practices may consider the implementation of additional mini-fellowships to improve proficiencies and bolster the confidence of new graduates prior to independent practice (22).
Our study is not without limitations. Our study is retrospective in design, utilizing surgical case volume data spanning 2 years from a single tertiary care center in Upstate, New York. As such, our findings may not be representative of orthopaedic surgical volumes in other geographic areas where the prevalence of COVID-19 and degree of hospital and state restrictions may have varied. Multicenter data collection is warranted to thoroughly assess the impact of the COVID-19 pandemic on orthopaedic surgical case volume. Despite these limitations, our analysis provides valuable data for orthopaedic surgeons by demonstrating the significant impact of the COVID-19 pandemic on surgical case volumes. Orthopaedic surgeons and hospital systems may use our study to compare the effects of the pandemic within their own practices, and to conceptualize approaches to limit the impact if similar government-imposed restrictions occur in the future.
Conclusions
The COVID-19 pandemic rapidly disrupted orthopaedic surgical volume, but since April 2020, we have observed a robust recovery largely due to a backlog in cases and furloughs at smaller regional centers. The results of our study are likely similar to those that were experienced throughout the country, especially in areas had COVID-19 related restrictions on elective procedures. Distressed healthcare organizations will likely consolidate further increasing surgical volume at large tertiary care centers. Additionally, orthopaedic residents may be adversely affected due to the lower volume of inpatient surgical candidates and the lack of access to ambulatory surgery centers. In conclusion, orthopaedic surgeons should be mindful of these new trends and plan accordingly prior to ratifying new agreements.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-16/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-16/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-16/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-23-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Albany Medical Center Institutional Review Board (IRB No. 00007321) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533-4. Erratum in: Lancet Infect Dis 2020;20:e215. [Crossref] [PubMed]
- Chang Liang Z, Wang W, Murphy D, et al. Novel Coronavirus and Orthopaedic Surgery: Early Experiences from Singapore. J Bone Joint Surg Am 2020;102:745-9. [Crossref] [PubMed]
- Parvizi J, Gehrke T, Krueger CA, et al. Resuming Elective Orthopaedic Surgery During the COVID-19 Pandemic: Guidelines Developed by the International Consensus Group (ICM). J Bone Joint Surg Am 2020;102:1205-12. [Crossref] [PubMed]
- Anoushiravani AA, Barnes CL, Bosco JA 3rd, et al. Reemergence of Multispecialty Inpatient Elective Orthopaedic Surgery During the COVID-19 Pandemic: Guidelines for a New Normal. J Bone Joint Surg Am 2020;102:e79. [Crossref] [PubMed]
- CMS Adult Elective Surgery and Procedures Recommendations [Internet]. U.S. Centers for Medicare and Medicaid Services. 2020 [cited 2020 May 1]. Available online: https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf
- Service BC, Collins AP, Crespo A, et al. Medically Necessary Orthopaedic Surgery During the COVID-19 Pandemic: Safe Surgical Practices and a Classification to Guide Treatment. J Bone Joint Surg Am 2020;102:e76. [Crossref] [PubMed]
- Phillips MR, Chang Y, Zura RD, et al. Impact of COVID-19 on orthopaedic care: a call for nonoperative management. Ther Adv Musculoskelet Dis 2020;12:1759720X20934276.
- Lanham NS, Bockelman KJ, McCriskin BJ. Telemedicine and Orthopaedic Surgery: The COVID-19 Pandemic and Our New Normal. JBJS Rev 2020;8:e2000083. [Crossref] [PubMed]
- Temesgen ZM, DeSimone DC, Mahmood M, et al. Health Care After the COVID-19 Pandemic and the Influence of Telemedicine. Mayo Clin Proc 2020;95:S66-8. [Crossref] [PubMed]
- Wong JSH, Cheung KMC. Impact of COVID-19 on Orthopaedic and Trauma Service: An Epidemiological Study. J Bone Joint Surg Am 2020;102:e80. [Crossref] [PubMed]
- Wright EV, Musbahi O, Singh A, et al. Increased perioperative mortality for femoral neck fractures in patients with coronavirus disease 2019 (COVID-19): experience from the United Kingdom during the first wave of the pandemic. Patient Saf Surg 2021;15:8. [Crossref] [PubMed]
- Thakrar A, Chui K, Kapoor A, et al. Thirty-Day Mortality Rate of Patients With Hip Fractures During the COVID-19 Pandemic: A Single Centre Prospective Study in the United Kingdom. J Orthop Trauma 2020;34:e325-9. [Crossref] [PubMed]
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. Erratum in: Lancet 2020;395:1038. [Crossref] [PubMed]
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) - China, 2020. China CDC Wkly 2020;2:113-22.
- Chang D, Lin M, Wei L, et al. Epidemiologic and Clinical Characteristics of Novel Coronavirus Infections Involving 13 Patients Outside Wuhan, China. JAMA 2020;323:1092-3. [Crossref] [PubMed]
- Anoushiravani AA, O'Connor CM, DiCaprio MR, et al. Economic Impacts of the COVID-19 Crisis: An Orthopaedic Perspective. J Bone Joint Surg Am 2020;102:937-41. [Crossref] [PubMed]
- Pirracchio R, Mavrothalassitis O, Mathis M, et al. Response of US hospitals to elective surgical cases in the COVID-19 pandemic. Br J Anaesth 2021;126:e46-8. [Crossref] [PubMed]
- Mead M, Atkinson T, Srivastava A, et al. The Return on Investment of Orthopaedic Fellowship Training: A Ten-year Update. J Am Acad Orthop Surg 2020;28:e524-31. [Crossref] [PubMed]
- Kogan M, Klein SE, Hannon CP, et al. Orthopaedic Education During the COVID-19 Pandemic. J Am Acad Orthop Surg 2020;28:e456-64. [Crossref] [PubMed]
- Plancher KD, Shanmugam JP, Petterson SC. The Changing Face of Orthopaedic Education: Searching for the New Reality After COVID-19. Arthrosc Sports Med Rehabil 2020;2:e295-8. [Crossref] [PubMed]
- Culp BM, Frisch NB. COVID-19 Impact on Young Arthroplasty Surgeons. J Arthroplasty 2020;35:S42-4. [Crossref] [PubMed]
Cite this article as: Anoushiravani AA, Kalyanasundaram G, Kuna M, Murasko M, Carroll J, Mulligan MT. Effect of coronavirus disease 2019 (COVID-19) on orthopaedic surgical volume. J Hosp Manag Health Policy 2023;7:4.

