
Expeditious formation of London Health Sciences Centre (LHSC) adult ground critical care transport team in aid of 3rd wave coronavirus disease 2019 (COVID-19) pandemic in Ontario, Canada
Highlight box
Key findings
• A pandemic such as coronavirus disease of 2019 (COVID-19) resulted the highest number of intensive care unit (ICU) admissions in Toronto, Canada which needed to decant to other local and regional hospitals to offload the burden in the ICUs.
• A clear mission goal and organizational accountability are required to organize an expeditious Critical Care Ground Transport (CCGT) team.
• Hospital senior leadership support is a must to expedite mandatory risk and safety assessments and mobilize required resources in the hospital and community.
What is known and what is new?
• Ornge, a government operated ground and air ambulance can be overwhelmed with critical care patient transport during a pandemic.
• Hospitals with adequate resources can establish own CCGT to assist in decanting critical care patients utilizing the Strengths, Weaknesses, Opportunities and Threats analysis (SWOT) to determine its potential to mobilized a CCGT with a clear mission goal and organizational accountability.
What is the implication and what should change now?
• Pandemic can overwhelm ICU care such as limited beds, ventilators, pharmaceutical agents and healthcare providers can result in increasing morbidity and mortality.
• Hospitals leadership needs to liaise with the provincial and municipal governments health authority; provincial or regional ground and air ambulance organization to establish multilateral cooperation and collaboration to maximize resources for patient care in preparation prior to a pandemic.
• Hospitals needs to maintain high quality CCGT members with strong clinical and communication skills; prior critical care transport experiences; ability to work well in a mobile enclosed platform and provide well maintained transport equipment.
Introduction
The Province of Ontario, Canada, experienced three waves of coronavirus disease of 2019 (COVID-19) infections since the declaration of the pandemic by the World Health Organization (WHO) on March 11, 2021 (1). The first wave in the spring to summer of 2020, the majority of deaths were among residents of long-term care facilities (2). A second state of emergency from January 12, 2021 till early March was influenced by the post-holiday surge of new COVID-19 infections (3). By mid-March 2021, a third wave resulted in the highest number of intensive care unit (ICU) admissions in Ontario since the start of the pandemic (4).
Ornge, formally known as Ontario Air Ambulance Corporation, is a not-for-profit organization that provides air (rotary and fixed wings) and ground ambulance services for critical and non-critical care patients in Ontario (5). As the number of ICU COVID-19 patients rose, Toronto and surrounding hospitals quickly became overwhelmed. The Ontario Critical Care COVID-19 Command Centre urgently needed to offload patients from overburdened ICUs to those with available capacity (6). In response to the increasing demand, Ornge gradually expanded their critical care transport for air and land by 300% by April 7, 2021. However, this effort was not enough to offload the burdens of ICUs in a timely manner (7). An appeal for assistance came on April 8, 2021 from the Provincial Command Table and Ornge. London Health Sciences Centre (LHSC) in partnership with the Middlesex London Emergency Medical Services (ML-EMS) implemented a novel Critical Care Ground Transport (CCGT) team capable of transporting stabilized critically ill COVID-19 patients to the most appropriate hospital. The first transport took place on April 16, 2021.
We describe the operational process for the LHSC CCGT team and the characteristics of the twenty-two patients transferred between April 16, 2021–May 7, 2021.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was not obtained from the patients transferred for publication of this case series due to the retrospective nature of this study. No accompanying images were used for publication. Copies of written consent is not available. No personal information written in the manuscript.
Operationalization LHSC critical care transport team
On April 9, an ICU physician lead, a clinical nurse specialist (CNS) and a senior registered respiratory therapist (RRT) at LHSC began a Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis to determine its potential to mobilize a CCGT (8). A potential strategy and developed protocol proposed and approved by senior leadership on April 13. Two teams formed consisting of one critical care registered nurse (CCRN) partner with a dedicated RRT. The North American RRT is an integral part of inter-professional healthcare team and trained to assess, monitor, and treat individual patients with lung diseases or disorders. The skills involve the administration of oxygen, CPR, management of mechanical ventilation, administration of drug to the lungs, monitoring cardiopulmonary systems and measuring lung function. The CCRN and RRT members selected based on their strong clinical skills, advanced directives, prior critical care transport experiences, and ability to work well in a small team and in a mobile enclosed platform. Each team was scheduled to provide coverage from 0700–1900, 7-day a week, and on April 15, the newly formed CCGT completed their orientation. One transport per day planned to move patients west from Toronto to LHSC and surrounding hospitals or from LHSC to facilities west of London to accommodate additional inflow from Toronto. An ICU consultant or ICU fellow in training to care and mange patients with potential adverse events that may occur during a transport supported each team. Travel duration to and from LHSC were within 2–3 hours each way. This time limit was set by the constraint of a single M-tank carried in the ambulance, with the supply duration dependent on the oxygen flow rate.
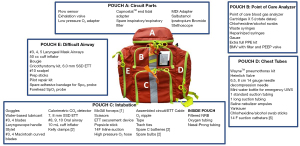
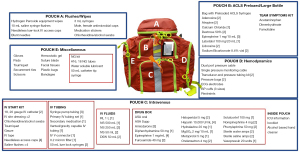
In addition to the standard ground ambulance equipment (Lifepak defibrillator/pacemaker; suction), the team brought equipment familiar to the team the Hamilton T1 portable mechanical ventilator with low pressure oxygen (LPO) mode enabled; Philips IntelliVue X3 monitor with electrocardiogram (ECG), oxygen saturation (SpO2) and 2 pressure cables; 4 Braun syringe pumps and 1 Baxter Sigma Spectrum infusion pump. Two Statpacks G3 Perfusion backpacks were used to carry disposable respiratory and cardiovascular supplies (Figures 1,2).
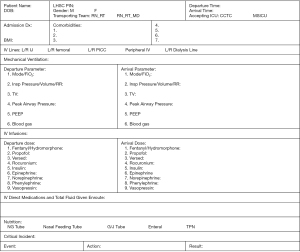
At 0700–0730, Ornge provided daily assignment. The on-call team contacted the sending facility to assess patient transportability (Figure 3). The inclusion criteria for transportation were ≥18 years old, COVID-19 positive and mechanically ventilated. The exclusion criteria for transportability mirrored Ornge operational criteria, which included fraction of inspired oxygen (FiO2) ≥70%, positive end-expiratory pressure (PEEP) ≥15 cmH2O, flow rate ≥15 liter/min, prone in the last 24-hour, on inhaled nitric oxide, patient greater than 84 cm wide and 272 kg, and hemodynamic instability that could not be stabilized by medications. Prior to departure, at 0800–0830, a ground ambulance from Middlesex London EMS with two primary paramedics awaits at the base hospital and review with the team members supplies and safety checklists.

Other transport documentations in addition to patient transportability created such as handover and Doctor of Medicine (MD) in-transit documents (Figures 4,5). The CCRN and RRT documentation initially consisted of in-hospital documentation and graphic records. However, the CCRN switched to timed progress note entries on a separate progress sheet at every 30-minute interval for ease of recording during transport. The progress sheet handed to the receiving nurse at final destination.

After each completed transport, the CCGT and paramedic team debriefed with the project leader using a tool developed to review critical incidents, communication, team role, personal protective equipment (PPE) integrity, clinical concerns, readiness of sending and receiving facilities. Issues identified and addressed before the next transport and checklists modified as required on an ongoing basis. Upon returning to home base, the team members would sanitize all equipment and replenish transport supplies. Some of the lessons learned from the debrief were:
- To minimize equipment failure during transportation, the CCTG team to perform a full equipment and battery check prior to departure from the sending hospital ICU.
- Streamline documentations. CCRN and RRT to decide the most efficient and comprehensive documenting patient’s hemodynamic and respiratory parameters.
- Support effective communication environment between team member by encouraging feedback, ideas and suggestions.
- Contact patient’s family members to ensure they know the patient to be transported outside of their home hospital and to provide them with the location and contact phone number of the receiving hospital.
Patients transported April 16–May 13, 2021:
April 16–May 7, 2021, Ornge requested twenty-five transports. Twenty-four were COVID-19 positive and all were mechanically ventilated. Twenty-two patients accepted for transport and three declined. Of these, two has escalating FiO2 requirement and a third required dialysis, which was not available at the receiving hospital. The CCGT team transported patients from six Toronto west hospitals of which seven patients went to the Critical Care Trauma Centre (CCTC)-Victoria Campus; two patients to the Medical-Surgical Intensive Care Unit (MSICU)-University Campus and three patients each to Woodstock, Stratford and St-Thomas hospitals. During this period, LHSC continued to receive high acuity patients directly via Ornge and operated at a surge capacity of 130%. The LHSC ICUs needed to decant COVID-19 patients in their units to accept more backlog from the Toronto region. The CCGT team decanted from CCTC and MSICU, seven and three patients to hospitals west of London Middlesex region.
Patient characteristics in Table 1 describes older males were transported than females, while females transported had a higher body mass index (BMI). The transporting time from the sending hospital to the receiving hospital was less than 2-hour.
Table 1
| Patient characteristics | Value (N=22) |
|---|---|
| Age (years), median (IQR) | 59.5 [36–82] |
| BMI (kg/m2), median (IQR) | 29.82 (19.27–36.31) |
| Sex, N (%) | |
| Male | 14 (63.64) |
| Female | 8 (36.64) |
| Comorbidities, N (%) | |
| Diabetes | 9 (40.91) |
| Hypertension | 10 (45.45) |
| Dyslipidemia | 7 (31.82) |
| Asthma | 1 (4.55) |
| CHF | 1 (4.55) |
| Renal failure | 4 (18.18) |
| Obesity, BMI >30 | 10 (43.48) |
| Minutes of transport (minutes), median (IQR) | 113.50 (80–180) |
| PaO2:FiO2 prior to transport, median (IQR) | 192.5 (86.67–425) |
| PaO2:FiO2 on arrival, median (IQR) | 180.18 (100.83–454.29) |
| PaCO2 prior to transport, median (IQR) | 50.50 (23–87) |
| PaCO2 on arrival, median (IQR) | 52.05 (27–113) |
| Modes of ventilation, N (%) | |
| Departure | |
| AC-PC | 13 (59.09) |
| AC-VC | 5 (22.73) |
| PSV | 4 (18.18) |
| Arrival | |
| AC-PC | 13 (59.09) |
| AC-VC | 5 (22.73) |
| PSV | 3 (13.67) |
| ASV | 1 (4.55) |
| Infusion medications, N (%) | |
| Departure | |
| Cisatracurium or rocuronium | 7 (31.82) |
| Fentanyl or hydromorphone | 19 (86.36) |
| Propofol or midazolam | 17 (77.27) |
| Norepinephrine | 12 (54.54) |
| Arrival | |
| Cisatracurium or rocuronium | 5 (22.73) |
| Fentanyl or hydromorphone | 18 (81.82) |
| Propofol or midazolam | 17 (77.27) |
| Norepinephrine | 12 (54.54) |
IQR, interquartile range; BMI, body mass index; CHF, congestive heart failure; PaO2, partial pressure of oxygen; FiO2, fraction of inspired oxygen; PaCO2, partial pressure of carbon dioxide; AC-PC, assist control-pressure control; AC-VC, assist control-volume control; PSV, pressure support ventilation; ASV, adaptive support ventilation.
Prior to departure from the sending facilities, the CCGT team requested pre-transport stabilization intervention on six patients. Two patients required stabilization for hypotension, systolic blood pressure (SBP) <90 mmHg and/or mean arterial pressure (MAP) <65 mmHg for more than 5-minute, while others required conversion of inhaled isoflurane to propofol infusion; insertion of a central line; clarification the goals of care and one cycle of peritoneal dialysis.
All twenty-one patients had the same mode of ventilation except one patient transitioned from pressure support ventilation (PSV) to adaptive support ventilation (ASV). In-vitro whole blood analyzer (ISTAT) utilized prior to arrival at destination found sixteen patients under-ventilated and five patients were over-ventilated. Although prone positioning within the preceding 24 hours considered a contraindication to transport, one patient who had been supinated within 2 hours of departure was successfully transported. Lower oxygen tank consumption than anticipated was also observed with the Hamilton transport ventilator; had continued transports been required, higher FiO2 threshold could have been supported.
One non-COVID-19 patient was in a neurological coma and the second patient was in the recovery phase did not require continuous infusions of narcotics and/or sedatives. Neuromuscular blockers were required in eight patients and vasopressors in ten patients. Patients transported from Toronto had higher acuity than those transported from LHSC.
Adverse events during critical care transport remains common and can be harmful to the patient. The incidence and severity of the events varies between published studies. This discrepancy resulted from the differences in the definition used for adverse events (9,10). We utilized the adverse event definition from Parmentier-Decrucq et al., Table 2 (11). Major related patient adverse event included five patients required an increase of FiO2 by 5–25% from baseline and one patient required FiO2 60% to 90%. However, two patients decreased FiO2 from 60% to 50%. There was no minor patient related adverse events. However, three equipment related incidents during interfacility transport, near misses related to electrical power. Battery charging failure occurred twice (syringe pump charging station and portable monitor). In each case, alternating current (AC) power was available which prevented an adverse event. A third incident occurred when there was an unrecognized loss of AC power in the ambulance. All device function was maintained because of adequate battery power. Each incidence occurred early on and corrective action was taken following daily debriefings. Additional checks including confirmation of ambulance and battery charge prior to departure was added to safety checklists.
Table 2
| Major patient-related adverse events during transport: |
| (I) Oxygen desaturation |
| (II) Extubation |
| (III) Accidental central venous catheter removal |
| (IV) Hemodynamic instability |
| (V) Increase vasopressor dose |
| Minor-patient related adverse events: |
| (I) Agitation |
| (II) Accidental nasogastric tube pulled out |
| (III) Vomiting |
| (IV) Peripheral venous catheter incident |
| (V) Central venous catheter incident |
| (VI) Arterial line incident |
| (VII) Accidental dislodging of urinary catheter |
| (VIII) Disconnection of endotracheal tube and airway equipment |
| Equipment-related incidents during transport: |
| (I) Incident with airway equipment (alarm, adjustment) |
| (II) Incident with monitor (battery, alarm) |
| (III) Incident with infusion pumps (battery, alarm) |
Discussion
COVID-19 pandemic continues to challenge hospital systems and ICU capacity around the globe. To overcome demand, the movement of critically ill patients from overburdened regions to facilities with available capacity may be required (12). We describe here our experience and lessons learned in the successful creation of an expeditionary CCGT team, safely completed twenty-two regional land transports. From our experience, the main principles in establishing an expeditionary transport team are the following:
- Conduct a SWOT analysis to identify potential resources, organizational impact and program feasibility (8).
- Establish a clear mission goal and organizational accountability.
- Obtain urgent senior leadership support in order to expedite mandatory risk and safety assessments and mobilize required resources.
- Establish clear communication channels between the transport team, emergency medical services and central dispatch (Ornge).
- Select experienced team members with strong clinical, organization and communication skills. Members have demonstrated ability to thrive in uncertain situations and establish solutions in extreme conditions. The ability to maintain composure while working without usual support systems is critical.
- Develop protocols and safety checklists to be implemented quickly and modified daily as new experiences arise.
- Utilize a rapid cycle improvement strategy such as Plan, Study, Do, Act (PSDA) cycle to provide ongoing quality and safety.
- Debrief daily and act on improvement opportunities immediately.
- Critical care transport is known to be difficult even during usual operations (13). It is imperative to establish clear communication with sending/receiving facility; choosing mode of transfer; pre-transfer stabilization and preparation; personnel accompanying the patient; equipment and monitoring required during the transfer; documentation and handover of the patient at the receiving facility (14,15). Evidence on clear transport principles and robust studies are lacking (16). A recent qualitative study published the importance of using checklists, special education programs, employing personnel interested in transport medicine which highlighted the need to standardize patient transports (15). Studies have also suggested that specific key qualities are required with the transport team members, such as collaborative teamwork, good problem-solving skills, mental agility, adequate physical fitness, compassion and excellent communication skills (14,17-19). It is accepted critically ill patients should be transferred by this specialized retrieval teams (20,21), but the composition, training and assessment of these teams is still an ongoing discussion (16). Certain skills and competencies have been noted to improve technical and non-technical performance during critical care transport; namely, previous ICU or deployment experience (22), flexibility, independence, critical thinking, problem solving, communication skills that enhance teamwork and crisis resource management (16,22). These research findings played a role in the development of our recommended principles.
In COVID-19 pandemic, many countries have shared their experience with transport of COVID-19 patients. Kuwait (23) and Singapore (24) demonstrated detailed planning that resulted in safe transport of mechanically ventilated patients, included broad categories such as transport equipment required, preparations before transport, the transport process, after arrival, and the post transfer decontamination. A set of transport guidelines developed in India to help mitigate the tremendous overburdening of the health care system (25). In France, a recent study involving 133 inter-hospital transfers of mechanically ventilated COVID-19 patients did not find an increase in ICU mortality but did report an increase in the median length of mechanical ventilation in the transferred group compared to the non-transferred group, 18 days [11–24] and 14 days [8–20], respectively (P=0.007) (26). This supports creation of expeditionary CCGT teams to help mitigate the management and spread of COVID-19 surge and future pandemics.
Conclusions
Third wave COVID-19 hit Toronto, Ontario, Canada by mid-March 2021 had a significant impact on its health system capacity such as ICU beds and mechanical ventilators. A novel Critical Care Ground Transport team was formed utilizing the SWOT analysis to determine its potential to mobilized a CCGT with clear mission goal and organizational accountability. Transport team members must have strong clinical and communication skills; prior critical care transport experiences; ability to work well in a mobile enclosed platform with a small team. Utilize a rapid cycle improvement strategy such as PSDA cycle to provide ongoing quality and safety with each completed patient transport.
Acknowledgments
We would like to acknowledge and thank the dedicated staff members of the Provincial Command Team, Ornge operational centre, and the senior leadership and paramedics of the Middlesex-London Emergency Medical Services for their encouragement, advice and resource support.
Funding: None.
Footnote
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-137/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-137/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- "WHO Director-General's opening remarks at the media briefing on COVID-19-11 March 20". World Health Organization (WHO).[cited March 11, 2020]. 2021. Available online: https://www.who.int/directorgeneral/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed June 2, 2021).
- “Ontario doesn't have a one-stop shop for information about COVID-19 deaths in long-term-care homes and hospitals”. The Toronto Star built its own". The star.com, Kenyon Wallace. [cited April 23, 2020]. Available online: https://www.thestar.com/news/gta/2020/04/23/ontario-doesnt-have-a-one-stop-shop-for-information-about-covid-19-deaths-in-long-term-care-homes-and-hospitals-the-toronto-star-built-its-own.html (accessed June 2, 2021).
- “Coronavirus: Ontario declares 2nd state of emergency, issues stay-at-home order". Global New, Ryan Rocca. [cited January 12, 2021]. Available online: https://globalnews.ca/news/7571036/ontario-new-restrictions-lockdown-coronavirus/ (accessed June 4, 2021).
- “Ontario now in third wave of COVID-19, province's hospital association says”. CTV News, Davidson, Sean. [cited March 15, 2021]. Available online: https://toronto.ctvnews.ca/ontario-now-in-third-wave-of-covid-19-province-s-hospital-association-says-1.5347940 (accessed June 4, 2021).
- Tien Homer, Sawadsky Bruce, Lewell Michael, Peddle Michael, Durham Wade. Critical care transport in the time of COVID-19. ORNGE Supplement CJEM 2020;1-5: [Crossref] [PubMed]
- This is such a serious disease': Inside an ICU patient transfer as COVID-19 cases rise. CTV News, Avis Favaro. [cited April 9, 2021]. Available online: https://www.ctvnews.ca/health/coronavirus/this-is-such-a-serious-disease-inside-an-icu-patient-transfer-as-covid-19-cases-rise-1.5381715 (accessed June 4 2021).
- “This critical care paramedic worked a week of 12-hour shifts to help keep Ontario's ICUs from overflowing”. CBC Radio, White Coat, black art. [cited May 7, 2021]. Available online: https://www.cbc.ca/radio/whitecoat/this-critical-care-paramedic-worked-a-week-of-12-hour-shifts-to-help-keep-ontario-s-icus-from-overflowing-1.5990745 (accessed June 4, 2021).
- Siddiqui Ahsan. SWOT Analysis (or SWOT Matrix) Tool as a strategic Planning and Management Technique in the Health Care Industry and Its Advantages. Biomed J Sci & Tech Res 2021;40:32035-32042.
- Murata M, Nakagawa N, Kawasaki T, et al. Adverse events during intrahospital transport of critically ill patients: A systematic review and meta-analysis. Am J Emerg Med 2022;52:13-9. [Crossref] [PubMed]
- Parveez MQ, Yaddanapudi LN, Saini V, et al. Critical events during intra-hospital transport of critically ill patients to and from intensive care unit. Turk J Emerg Med 2020;20:135-41. [Crossref] [PubMed]
- Parmentier-Decrucq E, Poissy J, Favory R, et al. Adverse events during intrahospital transport of critically ill patients: incidence and risk factors. Ann Intensive Care 2013;3:10. [Crossref] [PubMed]
- Rodrigue, JP, Luke, T, and Osterholm, M. Transportation and pandemics. In: J.-P. Rodrigue (Ed.), Geography of transport systems, 5th edn. Routledge, New York, NY, USA, 456. 2020.
- Bourn S, Wijesingha S, Nordmann G. Transfer of the critically ill adult patient. BJA Educ 2018;18:63-8. [Crossref] [PubMed]
- Kulshrestha A, Singh J. Inter-hospital and intra-hospital patient transfer: Recent concepts. Indian J Anaesth 2016;60:451-7. [Crossref] [PubMed]
- Eiding H, Kongsgaard UE, Braarud AC. Interhospital transport of critically ill patients: experiences and challenges, a qualitative study. Scand J Trauma Resusc Emerg Med 2019;27:27. [Crossref] [PubMed]
- Droogh JM, Smit M, Absalom AR, et al. Transferring the critically ill patient: are we there yet? Crit Care 2015;19:62. [Crossref] [PubMed]
- Orr RA, Felmet KA, Han Y, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics 2009;124:40-8. [Crossref] [PubMed]
- Kwack WG, Yun M, Lee DS, et al. Effectiveness of intrahospital transportation of mechanically ventilated patients in medical intensive care unit by the rapid response team: A cohort study. Medicine (Baltimore) 2018;97:e13490. [Crossref] [PubMed]
- Myers JA, Powell DM, Psirides A, et al. Non-technical skills evaluation in the critical care air ambulance environment: introduction of an adapted rating instrument--an observational study. Scand J Trauma Resusc Emerg Med 2016;24:24. [Crossref] [PubMed]
- Belway D, Henderson W, Keenan SP, et al. Do specialist transport personnel improve hospital outcome in critically ill patients transferred to higher centers? A systematic review. J Crit Care 2006;21:8-17; discussion 17-8. [Crossref] [PubMed]
- Chang AS, Berry A, Jones LJ, et al. Specialist teams for neonatal transport to neonatal intensive care units for prevention of morbidity and mortality. Cochrane Database Syst Rev 2015;2015:CD007485. [Crossref] [PubMed]
- Jernigan PL, Wallace MC, Novak CS, et al. Measuring Intangibles: Defining Predictors of Non-Technical Skills in Critical Care Air Transport Team Trainees. Mil Med 2016;181:1357-62. [Crossref] [PubMed]
- Yousuf B, Sujatha KS, Alfoudri H, et al. Transport of critically ill COVID-19 patients. Intensive Care Med 2020;46:1663-4. [Crossref] [PubMed]
- Liew MF, Siow WT, Yau YW, et al. Safe patient transport for COVID-19. Crit Care 2020;24:94. [Crossref] [PubMed]
- Munjal M, Ahmed SM, Garg R, et al. The Transport Medicine Society Consensus Guidelines for the Transport of Suspected or Confirmed COVID-19 Patients. Indian J Crit Care Med 2020;24:763-70. [Crossref] [PubMed]
- Painvin B, Messet H, Rodriguez M, et al. Inter-hospital transport of critically ill patients to manage the intensive care unit surge during the COVID-19 pandemic in France. Ann Intensive Care 2021;11:54. [Crossref] [PubMed]
Cite this article as: Kao R, Dave C, Risk M, St. John M, Hewitt J, Ballantyne S, Stephens M, Morgan B. Expeditious formation of London Health Sciences Centre (LHSC) adult ground critical care transport team in aid of 3rd wave coronavirus disease 2019 (COVID-19) pandemic in Ontario, Canada. J Hosp Manag Health Policy 2023;7:6.

