Physicians’ satisfaction with the use of teleconsultation in France
Introduction
Since the coronavirus disease 2019 (COVID-19) pandemic (1), the use of telehealth has surged as healthcare professionals have sought to safely deliver healthcare. Healthcare systems have had to adjust the method of medical care for patients by using methods that avoid physical contact. Teleconsultation helps provide necessary care to patients while being at the same time a solution for minimizing the transmission risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of 2019, the number of teleconsultation has increased from 500,000 to 1.3 million in 2021 in France (2). During the first lockdown in 2020, one in two doctors used telemedicine at least once (3). Telemedicine was initially recognized in France in 2009 as a legal form of medical service delivery that enables communication between healthcare professionals and patients (4). Today, the following five medical acts of telehealth are recognized by French law as (5): teleconsultation, tele-expertise, tele-assistance, remote monitoring, and medical regulation. For the past few years, Toulouse University Hospital has used a digital application, Teleo, available to its practitioners for teleconsultation (https://www.esante-occitanie.fr/). Teleo is a secure regional platform dedicated to telehealth practice, including remote consultation. This digital tool allows an audiovisual exchange between the doctor and the patient. Teleo also allows the exchange of documents and messages. Between 2019 and 2020, the number of teleconsultations at Toulouse University Hospital increased from 200 to 24,200. Its evolution was marked by two steps: in the first step, and given the emergency context, physicians had the possibility to use all digital tools that allow remote contact with the patient, including telephone calls and social networks such as WhatsApp and Teleo. In the second step, physicians increasingly use Teleo. Currently, the use of remote consultation in Toulouse University Hospital has decreased, probably due to the fall of COVID-19 cases in France. Since the COVID-19 pandemic, interest in the use of telehealth services by both physicians and patients has increased (6).
Despite the increase in telemedicine in recent years, few studies have assessed physician satisfaction and the obstacles they may encounter when dealing with remote consultations. These few studies did not analyze many of the factors that may have correlation with physician satisfaction, such as the profile of patients eligible for teleconsultation and the financial aspect of telemedicine practice (7). A review of the literature including 37 studies assessing satisfaction with telehealth practice revealed that the research designs used in the studies were less robust, with all studies using primary data to assess physician satisfaction, but only one study providing any type of multivariate analysis of physician satisfaction with telehealth (8).
For these reasons, it is essential to study the satisfaction and perspectives of physicians when using teleconsultation and to further analyse the factors that may have correlation with its practice.
Objectives
The objective of this study is to assess physicians’ satisfaction with teleconsultation and to identify factors that might influence its use. The secondary objective is to identify the advantages and disadvantages of teleconsultation. We present the following article in accordance with the SURGE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-76/rc).
Methods
Study design
A descriptive cross-sectional survey with a self-administered questionnaire was conducted at Toulouse University Hospital in June 2021.
This study was approved by Toulouse University Hospital and we confirm that ethic requirements were totally respected in the report. This study is cover by the MR-004 (CNIL number: 2206723 v 0). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all the participants.
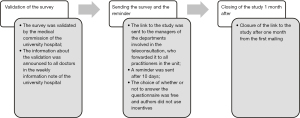
Surveys were sent to all physicians working in various departments in the Toulouse University Hospital: anesthesia-resuscitation, cardiovascular and metabolic, cephalic, digestive, children-mother-couple, infectious and tropical diseases, immunology, locomotor, urology, nephrology, plastic surgery and oncology by a link to their professional email. An email reminder was sent 10 days later by the pole managers (Figure 1). Physicians who had practiced teleconsultation at least once since the beginning of the COVID-19 pandemic were included in the study, regardless of the tool used: Teleo, traditional phone calls or social messaging like WhatsApp. This is verified in the questionnaire by a question: have you ever performed at least one teleconsultation with a remote patient in the last year? A negative answer excludes the respondent from the study. The response is only considered if the respondent has answered all the questions in the survey. If this is not the case, the respondent cannot submit their answers. We report that the practice of teleconsultation at the Toulouse University Hospital was mixed with face-to-face consultations. There was no day dedicated to teleconsultation.
Data collection
Data were collected through an online survey using Google Forms (Appendix 1). The survey was conducted in three sections. The first concerned socio-demographic data (age, job), the average number of consultations performed since the beginning of the COVID-19 crisis and the digital tools used for teleconsultation (Teleo, phone, WhatsApp). The second part concerned physicians’ opinions on teleconsultation, including a satisfaction evaluation with a scale derived from the Likert scale (very dissatisfied, dissatisfied, satisfied, very satisfied) and several questions evaluating physicians’ perspectives on telemedicine in terms of advantages, disadvantages, and limits when practicing remote consultation. The third part concerned the physicians’ expectations and projections of teleconsultation. In addition to satisfaction, obstacles and levers to the practice of teleconsultation, the questions also aimed to help us understand the typical profile of the patient eligible for teleconsultation and the doctors’ opinion on the hospital management needed to promote telemedicine.
The questions were drawn up with the referents for the development of digital health within the Toulouse University Hospital. These are doctors who are experts in telemedicine and actively participate in its development. All surveys were anonymized for data study.
For the statistical analysis, we split the physician’s responses into two groups: Satisfied if they responded “satisfied” or “very satisfied” on the Likert scale and the others were considered dissatisfied.
Statistical analysis
Quantitative data are presented as mean ± standard deviation (SD) if the distribution was normal and compared with Student’s t-test, if not by their medians [interquartile range (IQR)] and compared with the Mann-Whitney U test. The Kolmogorov-Smirnov test was used to verify the normality of the distribution. Categorical variables were described as percentages and compared using the chi-square test when the conditions of validity allowed it (theoretical numbers per cell were ≥5); if not, Fisher’s exact test was used. A 5% risk of error was used to analyze the results. Univariate analyses were performed to examine the associations between the two groups (satisfied and unsatisfied) and the metrics we used to assess physicians’ perceptions of telemedicine barriers and levers in the questionnaire. Binary logistic regression was performed in multivariate analyses to identify the predictive factors of the satisfaction rate. The satisfaction rate was considered as the dependent variable. Variables with a P value less than or equal to 20% were included in the univariate analysis. The significance level was set at 5%, and the strength of the association was estimated by calculating the odds ratio (OR) and its 95% confidence interval. Data were analyzed using the SPSS 20 software.
Results
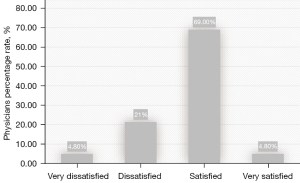
The overall response rate after the email reminder was 18.1% (145/800). The majority of the respondents were women (66.2%). The median age of the participants was 42 years, with extremes ranging from 28 to 67 years old (Table 1). Physicians report seeing an average of 20 patients per week, either face-to-face or remotely. Seventy-four percent of physicians were satisfied with teleconsultation, and the majority of physicians (67.6%) declared that teleconsultation was now part of their practice. Figure 2 presents physician satisfaction with teleconsultation.
Table 1
| Characteristics | N (%) |
|---|---|
| Number of teleconsultations in one year | |
| 1–10 | 21 (14.5) |
| 11–30 | 46 (31.7) |
| >30 | 78 (53.8) |
| Overall satisfaction | |
| Satisfied | 107 (73.8) |
| Not satisfied | 38 (26.2) |
| Teleconsultation was now part of their practice | |
| Yes | 98 (67.6) |
| No | 47 (32.4) |
| Most used teleconsultation tools | |
| Teleo direct | 114 (78.6) |
| Telephone | 62 (42.8) |
| Commercial apps: Skype, WhatsApp, FaceTime, etc. | 7 (4.8) |
Regarding the use of Teleo, 20% of teleconsultations ended in a phone call because of a technical problem. During their teleconsultation experience, physicians were globally satisfied with the ease of use (54%), sound (35%), image (23.4%), quality of connection (14.5%), and system reliability (absence of technical problems such as not being able to connect, not being able to hear the caller or not being able to have a visual exchange) (4.8%).
Physicians’ feedback on the advantages, indications, and limits of teleconsultation are described in Table 2. The main benefit of teleconsultation, according to 52.4% of respondents, is the possibility of saving money for health economics.
Table 2
| Questions and the most selected items | % |
|---|---|
| The advantages of teleconsultation cited were: | |
| The possibility of saving money for social security | 52.4 |
| Saving time for the physician | 41.4 |
| Improved patient care | 23.4 |
| The current limits of teleconsultation were: | |
| The lack of interoperability with the patient’s file (need for 2 screens) | 48.3 |
| The dehumanization of the doctor/patient relationship | 46.9 |
| The risk of medical errors is greater than in a face-to-face setting | 38.6 |
| The indications for which physicians performed the most teleconsultation were: | |
| COVID’s impact on the organization of care | 82.1 |
| Patients’ geographical distance and/or mobility restrictions and/or living in a nursing home | 66.2 |
| The indications for which senior physicians will propose a teleconsultation were: | |
| Patients’ geographical distance and/or mobility restrictions | 74.5 |
| Follow-up on complementary examinations (biology or radiology) | 68.3 |
| Treatment monitoring and its adaptation | 51.7 |
| The types of patients to whom physicians will or would never do a teleconsultation were: | |
| A poly trauma patient (traffic accident, fall from a high level, etc.) | 59.3 |
| An infant | 51.0 |
| A demented patient | 42.8 |
| A first consultation | 46.9 |
| A child | 21.4 |
| A pregnant woman | 17.9 |
The two main limitations to teleconsultation according to 48.3% and 46.9% of respondents respectively are the lack of interoperability with the patient’s file (need for 2 screens) and the dehumanization of the doctor/patient relationship. Regarding the practice of telemedicine according to the type of patients, the percentages of physicians who will never do teleconsultation are in decreasing order: never for a polytrauma patient (59.3%), never for an infant (51.0%), never for a demented patient (42.8%), never for a first consultation (46.9%), never for a child (21.4%) and never for a pregnant woman (17.9%).
According to our study, teleconsultation use will persist according 79.3% of the physicians. Physicians who will adopt teleconsultation wish to maintain mixed practice with face-to-face and remote consultations in 53.8% of cases. The duration of teleconsultations should be similar to that of physical consultation (15–20 minutes) in 51.7% of cases.
The univariate analysis (Table 3) showed that the increase in physician satisfaction was associated with several factors such as thinking that teleconsultation can save physicians time and that it improves patient care.
Table 3
| Factors | Satisfaction | P value | OR (95% CI) | |
|---|---|---|---|---|
| Yes, n (%) | No, n (%) | |||
| Gender | 0.407 | – | ||
| Male | 35 (71.4) | 14 (28.6) | ||
| Female | 74 (77.1) | 22 (22.9) | ||
| Age | 0.441 | – | ||
| <40 years | 43 (70.5) | 18 (29.5) | ||
| ≥40 years | 64 (76.2) | 20 (23.8) | ||
| Teleconsultation is now part of their practices | ≤10–3 | 7.430 (3.279–16.835) | ||
| Yes | 85 (86.7) | 13 (13.3) | ||
| No | 22 (46.8) | 25 (53.2) | ||
| Teleo as the most chosen teleconsultation tool | 0.054 | – | ||
| Yes | 89 (77.4) | 26 (22.6) | ||
| No | 18 (60.0) | 12 (40.0) | ||
| The telephone as the most chosen teleconsultation tool | 0.003 | 0.321 (0.149–0.693) | ||
| Yes | 38 (61.3) | 24 (38.7) | ||
| No | 69 (83.1) | 14 (16.9) | ||
| A tool for the general public: Skype, WhatsApp, FaceTime, etc. as the most chosen teleconsultation tool | 0.462 | – | ||
| Yes | 6 (85.7) | 1 (14.3) | ||
| No | 101 (73.2) | 37 (26.8) | ||
| Time saving for the doctor as an advantage of teleconsultation | 0.028 | 2.45 (1.086–5.553) | ||
| Yes | 50 (83.3) | 10 (16.7) | ||
| No | 57 (67.1) | 28(32.9) | ||
| The possibility of benefice for economic public health | 0.063 | – | ||
| Yes | 61 (80.3) | 15 (19.7) | ||
| No | 46 (66.7) | 23 (33.3) | ||
| Improving patient care as an advantage of telemedicine | 0.008 | 4.759 (1.362-16.624) | ||
| Yes | 31 (91.2) | 3 (8.8) | ||
| No | 76 (68.5) | 35 (31.5) | ||
| Dehumanization of the relationship between doctor and patient as a brake on telemedicine | 0.001 | 0.253 (0.113–0.564) | ||
| Yes | 41 (60.3) | 27 (39.7) | ||
| No | 66 (85.7) | 11 (14.3) | ||
| Non-adherence of patients as a brake on telemedicine | 0.131 | – | ||
| Yes | 21 (63.6) | 12 (36.4) | ||
| No | 86 (76.8) | 26 (23.2) | ||
| Risks of medical errors of greater than in person as a brake on telemedicine | 0.014 | 0.39 (0.18–0.83) | ||
| Yes | 35 (62.5) | 21 (37.5) | ||
| No | 72 (80.9) | 17 (19.1) | ||
| Tools not relevant or not efficient as a brake on teleconsultation | 0.001 | 0.274 (0.126–0.598) | ||
| Yes | 25 (55.6) | 20 (44.4) | ||
| No | 82 (82.0) | 18 (18) | ||
| Lack of interoperability with the patient file as a brake on teleconsultation | 0.896 | – | ||
| Yes | 52 (74.3) | 18 (25.7) | ||
| No | 55 (73.3) | 20 (26.7) | ||
| Satisfaction with the ease of use during the teleconsultation | 0.001 | 4.28 (1.91–9.56) | ||
| Yes | 68 (86.1) | 11 (13.9) | ||
| No | 39 (59.1) | 27 (40.9) | ||
| Satisfaction with the sound quality during the teleconsultation | 0.315 | – | ||
| Yes | 40 (80.0) | 10 (20.0) | ||
| No | 67 (70.5) | 28 (29.5) | ||
| Satisfaction with the image quality during the teleconsultation | 0.195 | – | ||
| Yes | 28 (82.4) | 6 (17.6) | ||
| No | 79 (71.2) | 32 (28.8) | ||
| Satisfaction with the quality of the connection during the teleconsultation | 0.06 | – | ||
| Yes | 19 (90.5) | 2 (9.5) | ||
| No | 88 (71.0) | 36 (29) | ||
| Satisfaction with the reliability of the system (no technical problem) during the teleconsultation | 0.673 | – | ||
| Yes | 6 (85.7) | 1 (14.3) | ||
| No | 101 (73.2) | 37 (26.8) | ||
CI, confidence interval; OR, odds ratio.
Using the telephone as the most chosen teleconsultation tool significantly reduces satisfaction (P=0.003).
The other barriers identified in our questionnaire that significantly reduce physician satisfaction are the belief that telemedicine dehumanizes the physician-patient relationship and that it increases the risk of medical errors.
Multivariate analysis showed that physicians’ satisfaction has a statistically significant correlation with the use of the telephone as a teleconsultation tool, which reduces physician satisfaction (P=0.018), the economic public health value (P=0.036), and the usability of the teleconsultation tool (P=0.037) (Table 4).
Table 4
| Factors | P value | OR (95% CI) |
|---|---|---|
| The phone as the most common tool of teleconsultation | 0.018 | 0.313 (0.119–0.819) |
| After the COVID-19 crisis, teleconsultation will persist in the practice | ≤10−3 | 5.35 (2.110–13.583) |
| The possibility of benefice for economic public health | 0.036 | 2.690 (1.067–6.780) |
| Tools not relevant or not efficient as a brake on teleconsultation | 0.008 | 0.281 (0.109–0.722) |
| Satisfaction with the ease of use of the tool dedicated to teleconsultation | 0.037 | 2.793 (1.064–7.333) |
CI, confidence interval; COVID-19, coronavirus disease 2019; OR, odds ratio.
Discussion
The overall satisfaction rate of the teleconsultation practice was 73.8%.
In our study, we found that the majority use of the telephone to perform teleconsultation decreased physician satisfaction. We also found that physician satisfaction was increased if they thought the socioeconomic impact of telemedicine was beneficial and if they found easy the use of the digital tool dedicated to the practice of telemedicine.
Use of teleconsultation
The overall satisfaction rate with teleconsultation was 73.8% in our study, which was similar to a study conducted by the Agency for Digital Health among a representative sample of 254 doctors practicing throughout France (116 general practitioners and 138 specialists), where 72% of physicians had a good opinion of telemedicine (9). An integrative review (10) assessed clinicians’ satisfaction with the use of teleconsultation, and four studies found a high level of satisfaction of 80% or more (11-14), while one study showed a healthcare provider satisfaction rate of 78% (15).
Several factors may influence physicians’ satisfaction with telemedicine. According to Demiris, physicians are most likely to be satisfied if they participate in its development (16). Satisfaction varies according to the physician’s specialty, as certain physicians are more suitable for remote consultation than others. This result is underlined by Kane et al., according to their study radiologists, and emergency physicians seem to use telemedicine more than other specialties (17). Nguyen et al. underline in their study that physicians who tended to be innovative were more likely to use telemedicine and were more satisfied regardless of teleconsultation ease of use (18).
In our study, the number of teleconsultations performed in one year was greater than 30 by physicians (53.8%). A study carried out in France by the National Health Agency from November 2019 to January 2020 showed that 21% of physicians performed more than 30 teleconsultations during a year (9). The difference in teleconsultation practices may be explained by the increase in teleconsultations in January 2020 due to the rise of COVID-19 cases.
At the beginning of the COVID-19 pandemic, all digital tools were authorized to perform remote consultations. However, quite rapidly the use of a secure telemedicine platform was required. The use of the telephone was authorized in the case of technical problems related to the platform. Among the digital tools of teleconsultation, 79.2% chose Teleo, followed by telephone (43%), notably when a technical problem occurred when using Teleo. Physicians preferred the use of Teleo because of the legal obligation to use an accredited platform for teleconsultation. Teleo was the only platform available for this practice at Toulouse University Hospital. In India, the tools used by pediatricians for teleconsultation were direct phone calls in 76.9% of the cases, followed by messages and WhatsApp calls in 71.8% (19). In Lebanon, the majority of physicians used WhatsApp (80%), followed by phone calls (67%) (20).
The technical problems encountered in our study are those encountered in telemedicine (connection, video, and sound quality). In Lyon (France), high satisfaction with sound and video quality had a significant impact on overall patient satisfaction (P=0.049) (21). As such, ensuring a good quality of audio, video equipment, and Internet connection is necessary to encourage physicians to use telemedicine (22). However, in our study, low satisfaction with sound and image quality did not affect global satisfaction. We believe that the high level of satisfaction with Teleo’s ease of use overcomes these drawbacks.
In our study, 20% of physicians reported a technical problem during teleconsultation. This percentage is lower than that reported by Monziols et al., who reported technical problems in approximately 50% of teleconsultations among general practitioners in France (23).
The duration of teleconsultation should be identical to face-to-face consultation, according to 51.7% of respondents, estimated at 20 minutes. Didier et al. reported similar results in 59.8% of physicians included in their study (24).
According to our study, after the COVID-19 crisis, physicians believe that teleconsultation will persist in their clinical practice (79.3%). Miner et al. found in a study conducted in the USA that 91% of a large multispecialty medical group of physicians plan to continue offering telemedicine services after the COVID-19 pandemic (25). This desire to persist in telemedicine use after the COVID-19 pandemic depends mainly on physicians’ satisfaction with telemedicine quality. This quality was evaluated using questions pertaining to satisfaction with telemedicine care.
Limits of teleconsultation
One of the main limitations of teleconsultations reported by physicians was the risk of dehumanization of the doctor-patient relationship (P=0.001) and the belief of a greater risk of medical errors than in a face-to-face setting (P=0.014). These limits are similar to those reported by the French Digital Health Agency. The majority of respondents felt that the doctor-patient relationship was dehumanized (46.6%). This percentage is lower than that reported by the French Digital Health Agency (68%) (9). This difference can be explained by the COVID-19 crisis, which encouraged physicians to practice more teleconsultation.
In a review, Solimini et al. described that legal and ethical issues of telemedicine include important aspects such as informed consent (information about the risks and benefits of remote therapy) (87%), malpractice and professional responsibility (70%), and professional–patient relationships (22%) (26).
Indeed, the doctor-patient relationship may be affected by the constant use of technological tools (27). A study performed in Toulouse in 2018 among general practitioners also described the risk of health dehumanization by teleconsultation (28).
Professor Mathieu-Fritz, a sociologist, has studied the link between teleconsultation and mental health. For him, the absence of “touch” by the doctor could diminish the carnal dimension, usually present in the therapeutic link. In its absence, the doctor loses a ritual element of greeting but also marks of proximity and moral support (29). There is certainly an impression of distance that goes against the link with the patient, but if physicians are aware of it, they will try to fight it (30).
In our study, physicians confirmed their reluctance to engage in teleconsultation in several situations. For example, 42.8% of the respondents in our study did not consider teleconsulting a patient with dementia.
Indeed, teleconsultation is unsuitable for all patients and situations. As reported by de Camargo Catapan et al., e-consultations may be less appropriate for people with learning disabilities, dementia, complex needs, and certain health problems, such as addiction, terminal illness, frail women, or the elderly. The use of e-mail was directly related to the educational level of patients, and the telephone seemed to be more appropriate for indigenous patients (31).
As teleconsultation appears to be the future of interconnected health, it is important to keep in mind that accessibility and ease of use must be technologically appropriate for all physicians and patients. Some clinicians are turned off by telemedicine because of the complexity of graphical interfaces. Similarly, the general population may be overwhelmed, especially if they are in a demographic group unfamiliar with similar technology (32). Therefore, patients must be properly trained to effectively use their devices and/or programs (33). The indications for teleconsultation must be pre-established to optimize the quality and efficiency of long-distance consultations. In our study, there was great variability in terms of medical indications for telemedicine according to the respondents. A total of 68.3% of physicians will propose teleconsultation for the follow-up of complementary examinations, while 11% will do so for pain management. According to Solimini et al., the perceived degraded quality in 30% of cases of remote medical consultation compared to standard face-to-face consultation is an ethical problem that hinders the rules of good practice (26).
Advantages and limitations
This study evaluated a diverse population of physicians working at one of the largest university hospitals in France. Several studies have evaluated the satisfaction of patients treated with telemedicine, but few have examined the satisfaction of physicians.
The overall response rate was 18.1%, which remained low and could represent a bias in extrapolating these results to the overall population of senior physicians.
There is a voluntary bias; physicians who participated in this study may have different characteristics from non-respondents who do not use teleconsultation very often.
Conclusions
Teleconsultation adoption by physicians is growing and may enhance traditional medicine practices. In the group studied in our survey, the majority of doctors were satisfied with the practice of telemedicine
In our study, doctors’ satisfaction with teleconsultation depends mainly on the digital tool used, which must be for them a platform adapted to the needs of teleconsultation. The resolution of technical and unpredictable connection problems is essential according to the physicians to ensure the promotion of telemedicine. In addition, the indications for teleconsultation should be pre-established in order to optimize the quality and efficiency of remote consultations. In our study, we also found that doctors support the use of telemedicine when they believe it is beneficial to the public health economy. It is therefore conceivable that better communication of the health economic benefits of telemedicine to physicians could help to increase their level of satisfaction with its practice.
Acknowledgments
The authors would like to thank Dr. France Lafisse for her contribution to this work.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-76/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-76/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-76/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-22-76/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by Toulouse University Hospital and we confirm that ethic requirements were totally respected in the above report. This study is cover by the MR-004 (CNIL number: 2206723 v 0) and informed consent was taken from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- COVID-19 – Chronologie de l’action de l’OMS [Internet]. Available online: https://www.who.int/fr/news/item/27-04-2020-who-timeline---covid-19
- Manus JM. Télémédecine hier, et aujourd’hui avec la Covid. Rev Francoph Lab 2021;2021:22-3. [Crossref] [PubMed]
- L’assurance maladie. Téléconsultation, une pratique qui s’installe dans la durée. Communiqué de presse du 16 septembre 2020. Available online: https://assurance-maladie.ameli.fr/presse/2020-09-16-cp-teleconsultation-anniversaire
- LOI n° 2009-879 du 21 juillet 2009 portant réforme de l’hôpital et relative aux patients, à la santé et aux territoires (1). 2009-879 juill 21, 2009. Available online: https://www.legifrance.gouv.fr/loda/id/JORFTEXT000020879475
- Décret n° 2010-1229 du 19 octobre 2010 relatif à la télémédecine. 2010-1229 oct 19, 2010. Available online: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000022932449
- American Medical Association, 2020. AMA Digital Health Research: Physician’s motivation and requirements for adopting digital health—adoption and attitudinal shifts from 2016 to 2019. Available online: https://www.ama-assn.org/system/files/ama-digital-health-study.pdf
- Saiyed S, Nguyen A, Singh R. Physician Perspective and Key Satisfaction Indicators with Rapid Telehealth Adoption During the Coronavirus Disease 2019 Pandemic. Telemed J E Health 2021;27:1225-34. [Crossref] [PubMed]
- Hoff T, Lee DR. Physician Satisfaction With Telehealth: A Systematic Review and Agenda for Future Research. Qual Manag Health Care 2022;31:160-9. [Crossref] [PubMed]
- Le baromètre de la Télémédecine de l’Agence du Numérique en Santé. Janvier 2020. Available online: https://esante.gouv.fr/sites/default/files/media_entity/documents/odoxa-pour-lans-et-le-mag-de-la-sante---barometre-telemedecine-vague-3---janvier-2021.pdf
- Andrews E, Berghofer K, Long J, et al. Satisfaction with the use of telehealth during COVID-19: An integrative review. Int J Nurs Stud Adv 2020;2:100008. Erratum in: Int J Nurs Stud Adv 2022 Dec;4:100092. [Crossref] [PubMed]
- Dobrusin A, Hawa F, Gladshteyn M, et al. Gastroenterologists and Patients Report High Satisfaction Rates With Telehealth Services During the Novel Coronavirus 2019 Pandemic. Clin Gastroenterol Hepatol 2020;18:2393-2397.e2. [Crossref] [PubMed]
- Rametta SC, Fridinger SE, Gonzalez AK, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology 2020;95:e1257-66. [Crossref] [PubMed]
- Svider PF, Setzen M, Ow R, et al. Incorporation of telemedicine by rhinologists: The COVID-19 pandemic and beyond. Am J Otolaryngol 2020;41:102567. [Crossref] [PubMed]
- Tenforde AS, Iaccarino MA, Borgstrom H, et al. Telemedicine During COVID-19 for Outpatient Sports and Musculoskeletal Medicine Physicians. PM R 2020;12:926-32. [Crossref] [PubMed]
- Gilbert AW, Billany JCT, Adam R, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual 2020;9:e000985. [Crossref] [PubMed]
- Demiris G. Examining health care providers’ participation in telemedicine system design and implementation. AMIA Annu Symp Proc 2006;2006:906. [PubMed]
- Kane CK, Gillis K. The Use Of Telemedicine By Physicians: Still The Exception Rather Than The Rule. Health Aff (Millwood) 2018;37:1923-30. [Crossref] [PubMed]
- Nguyen M, Waller M, Pandya A, et al. A Review of Patient and Provider Satisfaction with Telemedicine. Curr Allergy Asthma Rep 2020;20:72. [Crossref] [PubMed]
- Suryawanshi SP, Dhande PP, Deshmukh SR, et al. Pediatricians□ use and perception of tele-consultation services during coronavirus disease-19 pandemic. Natl J Physiol Pharm Pharmacol 2021;11:721-6. [Crossref]
- Helou S, El Helou E, Abou-Khalil V, et al. The Effect of the COVID-19 Pandemic on Physicians' Use and Perception of Telehealth: The Case of Lebanon. Int J Environ Res Public Health 2020;17:4866. [Crossref] [PubMed]
- Fieux M, Duret S, Bawazeer N, et al. Telemedicine for ENT: Effect on quality of care during Covid-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis 2020;137:257-61. [Crossref] [PubMed]
- Chavooshi B, Mohammadkhani P, Dolatshahi B. A Randomized Double-Blind Controlled Trial Comparing Davanloo Intensive Short-Term Dynamic Psychotherapy as Internet-Delivered Vs Treatment as Usual for Medically Unexplained Pain: A 6-Month Pilot Study. Psychosomatics 2016;57:292-300. [Crossref] [PubMed]
- Monziols M, Chaput H, Verger P et al. Trois médecins généralistes sur quatre ont mis en place la téléconsultation depuis le début de l’épidémie de Covid-19. Etudes et Résultats. 2020, n° 1162. Available online: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/ER%201162-te%CC%81le%CC%81consultation-BAT.pdf
- Didier M. Téléconsultation: l’opinion des médecins généralistes d’un territoire lorrain Etude quantitative réalisée auprès des médecins généralistes de Meuse et de la région de Toul. Université de Lorraine; 2015. Available online: https://hal.univ-lorraine.fr/hal-01733671/document
- Miner H, Fatehi A, Ring D, et al. Clinician Telemedicine Perceptions During the COVID-19 Pandemic. Telemed J E Health 2021;27:508-12. [Crossref] [PubMed]
- Solimini R, Busardò FP, Gibelli F, et al. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina (Kaunas) 2021;57:1314. [Crossref] [PubMed]
- Mian A, Khan S. Medical education during pandemics: a UK perspective. BMC Med 2020;18:100. [Crossref] [PubMed]
- Nadolny J, Rahuel C. La télémédecine: approches et propositions des médecins généralistes libéraux français. Etude qualitative menée auprès de médecins généralistes libéraux de l’ancienne région Midi-Pyrénées du mois de mai au mois d’août 2018. Université Toulouse III - Paul Sabatier; 2019. Available online: https://books.google.fr/books/about/La_t%C3%A9l%C3%A9m%C3%A9decine_approches_et_proposit.html?id=cbFLzQEACAAJ&redir_esc=y
- Mathieu-Fritz, A. Les téléconsultations en santé mentale. Reseaux n° 207, 123–164, 2018. Available online: https://shs.hal.science/halshs-01737364
- Slate.fr. Télémédecine, la solution aux déserts médicaux?. Slate.fr. 2018 [cité 4 août 2021]. Available online: http://www.slate.fr/sante/besoinsensante/episode-1-telemedecine-solution-desert-medicaux
- de Camargo Catapan S, Calvo MCM. Teleconsultation: an Integrative Review of the Doctor-Patient Interaction Mediated by Technology. Revista Brasileira de Educação Médica 2020;44:e002. [Crossref]
- Teoli D, Aeddula NR. Telemedicine. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2022.
- von Wangenheim A, Nunes DH. Creating a Web Infrastructure for the Support of Clinical Protocols and Clinical Management: An Example in Teledermatology. Telemed J E Health 2019;25:781-90. [Crossref] [PubMed]
Cite this article as: Kaissar S, Zara S, Fabrice F, Marion V, Jade B, Vincent M, Antoine P. Physicians’ satisfaction with the use of teleconsultation in France. J Hosp Manag Health Policy 2023;7:1.