
Reducing wait times to surgery—an international review
Introduction
There are wait times for health services (often seen as too long) in many countries, and are seen as a major challenge to many developed nations. In particular, long wait times for elective (i.e., non-emergent) surgical services have been the source of increased dissatisfaction among patients, impacting patient-centred care, and requiring health system decision-makers to develop policy actions to counter them. In 21 of 34 countries surveyed by the Organization for Economic Co-operation and Development (OECD) wait times was stated as either of high-priority or medium-high priority for their health systems (1). The main concern in most of these countries is around wait times for elective treatments; e.g., in Canada, wait times for hip and knee replacements are approximately 3 times as long as they are in Denmark (1).
A companion paper (submitted for publication) reported on approaches implemented in several countries targeting wait times from referral to first appointment with a specialist, also known as “wait time 1”. In this paper, approaches implemented to reduce wait times from the decision to perform surgery to the actual surgical service (wait time 2) are examined.
Methods
For this study, wait times were defined as the time from decision to perform surgery to when the surgery takes place (2,3). Information was obtained in two ways: (I) through interviews with key informants who were identified across Canada, and publicly funded health care systems in 13 countries that outranked Canada on performance measures related to access to selected surgery [Australia, Denmark, France, Germany, Israel, Italy, Netherlands, New Zealand, Norway, Sweden, Switzerland, UK, and the United States (Medicare/Medicaid)] (4,5); and (II) a scoping review of the literature (to identify additional approaches not reported in the interviews) following the Arksey O’Malley methodological framework (6). Complete details of these methods are provided in the companion paper.
Interviews
Multiple sources including referral from experts were used to identify potential interview participants. Additional candidates were obtained through websites of health authorities of health, relevant surgical associations, personal contacts in the international health technology assessment community, and recommendations from individuals already interviewed. Recruitment continued until saturation of information was reached. Because this study was part of a quality improvement project, ethical approval was not required.
Interviews were conducted over the phone with one researcher leading the interview and up to two others taking notes. Interview questions asked about approaches used to improve access to scheduled surgeries, program design and implementation. Participants’ responses were validated and analyzed to identify themes.
Scoping review
An experienced information specialist developed and validated the search strategy, which was applied to the following databases: Ovid MEDLINE®, Embase, the Cochrane library, CINAHL, EconLit and Web of Science. Search strategies were also developed to identify documents in the grey literature using the Google search engine, websites of ministries of health, health authorities and hospitals.
Documents were included if they: (I) described a method, system, policy or approach directly or indirectly intended to reduce wait times and (II) were in English or French. Documents were excluded if they described approaches targeting non-elective surgeries or transplants.
Two reviewers independently screened titles and abstracts and assessed the full-text documents against the eligibility criteria. In case of disagreement between reviewers, a third reviewer was consulted. Information was extracted using a standardized, pre-tested form.
Synthesis and quality appraisal of findings from the interviews and scoping review
Approaches were identified through both methods were separately analyzed for themes, each theme representing an approach. A common set of approaches was then compiled. Since wait times occur because of a mismatch of the demand for services and the supply of services to deliver them, the approaches identified were classified into supply-side strategies, demand-side strategies or both. For each approach, the quality and strength of evidence were assessed using categories from previous literature (7) and presented in Table 1. Findings from the synthesis of information were structured to comply with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) (8).
Table 1
| Quality appraisal criteria |
| Amount of evidence |
| Consistency of evidence |
| Certainty of evidence |
| Strength of evidence criteria |
| Consistent positive evidence of effectiveness* |
| Limited but promising evidence of effectiveness |
| Mixed evidence of effectiveness |
| Not possible to determine—no information on impact found |
| Not possible to determine—implemented alongside other approaches |
| Consistent negative evidence of effectiveness |
*, at least three sources of information presenting the same findings of their impact on wait times.
Results
The peer-reviewed search strategy identified 32,314 records, out of which 798 were retrieved for full-text review after removal of duplicates and title screening. Ultimately, 92 articles met the eligibility criteria (Figure 1). A total of 242 documents from the grey literature and 32 interviews from seventeen different countries were also included in the study (Table 2).
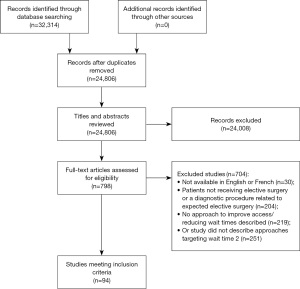
Table 2
| Characteristics | Publications, n [%] |
|---|---|
| Total | 366 [100] |
| Source of information | |
| Peer reviewed studies | 92 [25] |
| Grey literature | 242 [66] |
| Interview | 32 [9] |
| Region | |
| Australia | 58 [16] |
| Canada | 170 [46] |
| Denmark | 6 [2] |
| Finland | 1 [0] |
| France | 1 [0] |
| Hong Kong | 2 [1] |
| Ireland | 5 [1] |
| Israel | 4 [1] |
| Netherlands | 3 [1] |
| New Zealand | 14 [4] |
| Norway | 11 [3] |
| Portugal | 1 [0] |
| Spain | 6 [2] |
| Sweden | 13 [4] |
| Switzerland | 1 [0] |
| United Kingdom | 55 [15] |
| United States | 7 [2] |
| Multiple | 10 [3] |
| Specialty area | |
| Cardiothoracic | 12 [3] |
| ENT | 6 [2] |
| General surgery | 9 [2] |
| Gynecology | 1 [0] |
| Oncology | 14 [4] |
| Ophthalmology | 13 [4] |
| Orthopedic/neurosurgery | 52 [14] |
| Pediatrics | 3 [1] |
| Urology | 2 [1] |
| Vascular surgery | 1 [0] |
| Various | 252 [69] |
| Not reported | 2 [1] |
ENT, ear, nose and throat.
Table 3 provides details on 33 approaches targeting wait time 2 identified in interviews and the literature. Among them, 24 were supply-side strategies, 5 were demand-side strategies and 4 targeted both supply and demand. Fifteen approaches had consistent or limited but promising evidence supporting their effectiveness. The supplemental material (available at https://cdn.amegroups.cn/static/public/jhmhp-21-96-1.pdf) provides all references and detailed information regarding all approaches.
Table 3
| Approach, source of information, n (%) | Categories | Strength of evidence |
|---|---|---|
| Supply-side approaches | ||
| Expanded roles for non-physicians, n=16 (4%) | Non-physician-led surgery | Consistent positive evidence of effectiveness |
| Pre-admission assessments | ||
| Process improvement methodology, n=15 (4%) | LEAN | Consistent positive evidence of effectiveness |
| Six Sigma | ||
| LEAN/Six Sigma | ||
| Others | ||
| Publicly funded, privately delivered services, n=48 (13%) | Not applicable | Consistent positive evidence of effectiveness |
| Same-day surgery and discharge, n=18 (5%) | Not applicable | Consistent positive evidence of effectiveness |
| Standardized treatment pathways, n=16 (4%) | Not applicable | Consistent positive evidence of effectiveness |
| Streamlined pre-admission processes, n=18 (5%) | Centralized pre-admission clinics | Consistent positive evidence of effectiveness |
| Telephone pre-admission services | ||
| Targeted funding, n=60 (16%) | Elective procedures | Consistent positive evidence of effectiveness |
| Human resources | ||
| Infrastructure | ||
| Scheduling | ||
| Centralization of elective surgeries, n=14 (4%) | Centre dedicated to elective surgery | Limited but promising evidence of effectiveness |
| Centre dedicated to elective surgery at a hospital | ||
| OR dedicated to elective surgeries within a hospital | ||
| Centralized surgical scheduling, n=14 (4%) | Not applicable | Limited but promising evidence of effectiveness |
| Efficient use of ORs, n=9 (2%) | Parallel processing | Limited but promising evidence of effectiveness |
| Concurrent run ORs | ||
| Family doctors-led surgeries, n=3 (1%) | Not applicable | Limited but promising evidence of effectiveness |
| Fast-track programs, n=4 (1%) | Not applicable | Limited but promising evidence of effectiveness |
| Patient choice, n=36 (10%) | Hospital | Limited but promising evidence of effectiveness |
| Surgeon | ||
| Surgery date | ||
| Mobile surgical clinics, n=4 (1%) | Not applicable | Mixed evidence of effectiveness |
| Organization incentives, n=19 (5%) | Activity-based funding | Mixed evidence of effectiveness |
| Pay-for-performance | ||
| Disincentives | ||
| Non-financial incentives | ||
| Appointment reminders, n=1 (<1%) | Text | Not possible to determine—no information on impact found |
| Cancellation lists, n=5 (1%) | Not applicable | Not possible to determine—no information on impact found |
| Flex days, n=1 (<1%) | Not applicable | Not possible to determine—no information on impact found |
| Innovative surgical approaches, n=4 (1%) | Not applicable | Not possible to determine—no information on impact found |
| No-show policies, n=1 (<1%) | Not applicable | Not possible to determine—no information on impact found |
| Procedure rooms, n=1 (<1%) | Not applicable | Not possible to determine—no information on impact found |
| Pre-habilitation clinics, n=11 (3%) | Not applicable | Not possible to determine—implemented alongside other approaches |
| Provider incentives, n=3 (1%) | Financial incentives | Not possible to determine—implemented alongside other approaches |
| Non-financial incentives | ||
| Privately funded, privately delivered services, n=9 (2%) | Not applicable | Consistent negative evidence of effectiveness |
| Demand-side approaches | ||
| Prioritization of patients, n=47 (13%) | Not applicable | Consistent positive evidence of effectiveness |
| Regular validation of wait lists, n=7 (2%) | Not applicable | Consistent positive evidence of effectiveness |
| Subsidies for private health insurance or privately funded health insurance, n=2 (1%) | Not applicable | Not possible to determine—no information on impact found |
| Wait list management policies, n=2 (1%) | Not applicable | Not possible to determine—no information on impact found |
| Patient-targeted appropriateness initiatives, n=2 (1%) | Not applicable | Consistent negative evidence of effectiveness |
| Supply and demand approaches | ||
| Ongoing monitoring, analysis, and reporting of wait time and other outcomes data, n=55 (15%) | Not applicable | Not possible to determine—implemented alongside other approaches |
| Operations research and resource planning tools, n=12 (3%) | Not applicable | Not possible to determine—no information on impact found |
| Public reporting of wait times, n=19 (5%) | Not applicable | Not possible to determine—no information on impact found |
| Wait time targets, n=55 (15%) | Legally binding wait time targets or guarantees enforced through positive and negative incentives | Mixed evidence of effectiveness |
| Legally binding wait time targets or guarantees and mandatory offer of alternative provider enforced through negative or positive incentives | ||
| Legally binding wait time targets or guarantees and mandatory offer of alternative provider | ||
| Non-legally binding wait time targets or guarantees and offer of alternative provider | ||
| Non-legally binding wait time targets or guarantees | ||
ORs, operating rooms.
Expanded roles for non-physicians
Examples of expanded roles for non-physicians included performance of pre-admission services (interviews, education and pre-anesthesia assessment) by nurses. One study from the UK reported the median waiting time from referral to surgery dropped by a half after the introduction of a nurse-run pre-operative assessment for hernia (9).
Five examples of nurses performing biopsies, hysteroscopy, carpal tunnel syndrome procedures, and anesthesia during pacemaker implantation were identified (10-14). Specialists assisted nurses when needed and were able to focus on complex cases. Studies reported an improvement in wait times for the service provided by nurses (12,14) and low complication rates (12). In one study where nurses were in charge of low complexity cases, doctors were able to focus on cases that were more complex which, in turn, improved wait times (14). However, in one study, the hiring of nurses to perform tasks typically done by physicians received criticism from surgeons, who felt that there was already a nursing shortage and a lack of evidence that such an approach was cost-effective (12).
Process improvement methodology
Process improvement methodologies aimed to improve quality and efficiency of healthcare services. LEAN, Six Sigma or both were the approaches. LEAN refers to a set of methods and philosophies whose goal is to eliminate waste through an ongoing process. Six Sigma is a data-driven approach focusing on preventing defects.
Peer-reviewed studies and non-peer-reviewed documents described LEAN/Six Sigma applied in different medical areas and healthcare settings. They demonstrated that such methods improved one or more of the following factors: wait times (to surgery), wait list numbers, surgical volumes, case throughput, numbers of no-shows and costs (15-26). Neither LEAN nor Six Sigma were mentioned during interviews.
Publicly funded, privately delivered services
To increase surgical capacity, countries like Denmark, Australia, and Norway have provided publicly funded surgical services in private facilities through contractual arrangements as a means of quickly obtaining access to additional capacity. Across peer-reviewed studies, it was reported that the provision of publicly funded surgeries through private facilities resulted in a decrease in the number of patients on public waiting lists (27-29). However, in Scotland, it was eventually determined that the program offered poor value for money and contracts were terminated (29). Evidence from other sources also demonstrated increased surgical volumes (30,31) and reduced wait times (30,32,33). Some unintended consequences of this type of funding were reports of patients being charged extra operating costs (34) and an influx of more complex cases into the public system (35). While no impact on wait times was mentioned during interviews, one participant reported that the Auditor General from Canada recommended better accountability and management of privately delivered services.
Same-day surgery and discharge
Many public healthcare systems are making efforts to increase the use of same day surgery to reduce wait times by increasing efficiency. Surgeries performed are often “less complex” or of “lower acuity” and patients may need to meet certain medical eligibility criteria. Some programs ensure patients have the right supports in place at home first before approving them for same-day surgery and discharge.
Evidence consistently showed a reduction in wait times, more efficient use of resources, fewer cancellations due to bed shortages, and increased numbers of operations (36-38). In interviews, participants from Canada, Denmark and Netherlands described same-day surgeries but no impact on wait times was reported. However, one interviewee mentioned satisfaction from patients after joint replacement as long as they had someone helping them at home. Another participant also found great return on investment from a same-day mastectomy program.
Standardized treatment pathways
Standardized treatment pathways prescribe the care patients should receive from referral to treatment. They aim to reduce wait times by standardizing and streamlining patient care.
Documents and interviews reported that standardized treatment pathways significantly reduced all wait time measures from referral to surgical procedure with one source describing a reduction of 12% in waiting times from decision-to-treat to surgery (39-42). Other benefits of standardized pathways included reduction in length of hospitalization, costs and cancellation rates (39-41).
Streamlined pre-admission process
Streamlined pre-admission processes are designed to make the pre-admission process more efficient. At centralized pre-admission clinics, all pre-assessment services are provided in a single location to prepare patients for surgery and what to expect post-operatively. Streamlined pre-admissions can also be conducted via telephone for eligible patients to reduce burden of multiple travels.
Five peer-reviewed studies on pre-admission clinics were identified. The first examined a redesigned day-surgery centre in Norway, where patients cleared for elective surgery proceed directly to the laboratory for blood sampling and a drop-in anesthesia clinic for medical pre-assessment (43). The second study looked at the introduction of pre-operative consent clinics for patients with ear, nose and throat (ENT) issues 2 weeks prior to surgery to ensure their diagnostic tests are up-to-date (44). The third study examined the implementation of a pre-operative assessment clinic as part of a new direct-access day-case surgery process for general surgery. Patients were assessed by a nurse at the clinic 1 week before surgery (9). The fourth study reviewed the implementation of nurse-led multidimensional preoperative assessment for frail, older adults undergoing elective surgery (45). The fifth study reviewed the pre-admission process for cardiothoracic surgeries (16). The studies reported fewer cancellations (16,44,45) and a reduction in wait times for surgery (9,44,45). Other sources reported that cancellation rates decreased (46) and capacity increased (47).
Evidence on telephone pre-admission services was limited since the approach was implemented alongside other strategies. However, one source from Australia indicated that the service was more efficient and cost-effective (48).
Targeted funding
This is essentially a policy intervention whereby additional funds are made available to health authorities to increase the number of surgeries and work hours, improve infrastructure, and ensure that the necessary human resources are available to provide services in a timely manner. Across different sources, including one interview, targeted funding demonstrated reduced wait times and wait lists while also increasing the number of surgeries (49-54). However, this impact may not be sustained without continued funding (51).
Centralization of elective surgeries
To increase efficiency and quality of care, elective surgeries have been centralized in some jurisdictions through the establishment of dedicated operating rooms (ORs) or centres attached to or within hospitals. In general, dedicated centres only perform elective surgeries of low complexity. Thus, they need a robust process to select suitable patients.
One study reported on the centralization of low-complexity orthopedic surgery in British Columbia, Canada and found a decrease in the number of patients waiting longer than 26 weeks in the first 2 years. The waiting list also decreased in the first year, but slightly increased in the second year (49). The second study was on a prophylactic mastectomy program in which 5 ORs in an ambulatory centre were dedicated to the program once a month. The program successfully reduced wait times (55). Other sources reported reduced wait times following the centralization of cataract surgeries in Canada (56) and elective surgeries in England (57).
Centralized surgical scheduling
Central booking offices have been established to manage surgeons’ wait lists and schedule their surgeries. Offices may serve surgeons at a single hospital or several hospitals within a region. The approach aims to improve management of surgical waitlists and patient experience.
Evidence relating to the effectiveness was limited. One peer reviewed study examined the impact of an electronic surgical planning system for all elective surgeries in a Norwegian hospital (43). The system was implemented alongside an electronic referral system, development of a day-surgery centre, and redesign of the elective surgery care pathway. While the results suggested a reduction in cancellation rates and an increase in surgical volume, it was not possible to determine if these were attributable to the new scheduling system or other changes implemented at the same time (43). One unpublished report described a reduction in number of patients on the wait list after centralized scheduling was implemented alongside other strategies (58). One Canadian interviewee suggested that, while surgeons may resist giving up management of their wait lists and scheduling at first, most eventually appreciate central scheduling offices due to their positive impact.
Efficient use of ORs
Parallel processing has been used to reduce idle time by having patients sedated in one room while the OR is being cleaned and set-up. Concurrently run ORs (i.e., “swing” rooms or “flip-flop” rooms) allow surgeons to move between surgeries being performed in different ORs as the patients are ready for them. Both are viewed as innovative ways to increase OR efficiency.
One peer-reviewed study described a surgeon’s experience using parallel processing while performing hernia repairs at a hospital in the US (59). It reported that the approach significantly shortened induction and turnover times sufficiently (without compromising patent safety or satisfaction) to allow the addition of new operative cases. One document from Australia also reported improvements in efficiency, capacity, and cancellation rates, minimizing overruns with consequent overtime staff costs (60).
The literature from Canada and the US in different specialty areas reported increased OR efficiency with concurrent ORs (55,61,62) and improvements in wait times (55,63). However, one study found a limit at which the two-room model could not further increase efficiency (62). One interviewee also reported that, while efficiency increased, it was not enough to allow for additional procedures to be performed.
Family doctors-led surgeries
Family doctors in New Zealand, Ireland and the UK received training to provide low-complexity surgeries including general surgery, ENT procedures and vasectomies, respectively. According to one source, surgery performed by family doctors were appropriate and waiting times from referral to treatment improved (46). No further information on impact was found.
Fast-track programs
Fast-track programs establish preferential pathways for patients with suspected cancer, who once have diagnosis confirmed, undergo treatment within a pre-established timeframe.
Studies reported reduction in wait times from referral to first treatment (64,65), and from time of diagnosis to treatment (66). However, one study found the success of the program depended on specialists extending their work hours (65), and another reported most patients still exceeded the wait time targets (64). Fast track programs were not mentioned during the interviews.
Patient choice
Patients have the option to choose a hospital or surgeon with the shortest waiting times. In some jurisdictions, waiting times and other quality indicators were made available or patients had the option of choosing their surgery date in an effort to decrease anxiety and cancellations.
Two documents reported that patient choice of surgeon reduced wait times (39,67). One peer-reviewed study described reductions in wait times from referral to treatment after choice of hospital was introduced in the UK (68). One hospital in Norway allowed patients to choose their surgery date, but no information on impact was found (69). According to interviewees, the approach was implemented in some Canadian provinces, but no information on impact was found.
Mobile surgical clinics
Mobile surgical clinics are self-contained units that deliver services in geographically isolated areas or small towns that may lack access to healthcare providers. These clinics typically operate as one-stop shops, treating patients from referral to discharge, and are able to perform some minor surgical procedures.
Evidence of effectiveness from New Zealand and the United Kingdom was mixed. According to different sources, mobile clinics increased surgical capacity and allowed wait time targets to be met (70,71). One interviewee also informed that the service provided work force training for rural areas, but mobile clinics were clinically inappropriate for many patients. One study also found the quality of services provided was not assessed, and initially, many complications were reported. The study suggested mobile clinics made some staff at public hospitals obsolete by reducing volume of services at these facilities (72).
Organization incentives
Countries implement financial and non-financial incentives to encourage organizations to improve their services. Financial incentives can be further categorized into: activity-based funding, pay-for-performance, and disincentives. In activity-based funding, institutions are allocated funds based on the complexity of the patients (case-mix) and the type and volume of services they provide to the patients they serve. In pay-for-performance, the payment to an institution depends on it meeting pre-established benchmarks.
In 2000, England implemented a star rating system in which hospitals received rewards (greater autonomy) or sanctions (dismissal of managers) based on a set of indicators. One study reported positive outcomes after this policy (73). However, another study found many providers, while happy with the outcomes, experienced considerable pressure from the system (74).
In regard to activity-based funding, evidence from both peer-reviewed literature and one interview suggested that the approach increased surgical volumes and reduced wait times. However, in Denmark and Norway, complaints were reported about up-coding (i.e., reporting higher severity to increase income). In Denmark, it was also suggested that the process led to budgetary uncertainties (75,76). Finally, one unpublished document reported a decrease in number of patients waiting more than 90 days for treatment after introduction of pay-for-performance in Sweden (77).
Appointment reminders for surgeries
Appointment reminders comprised the use of text messages to send reminders to patients of their surgery in order to reduce cancellations. In some countries, such reminders are automated. Patients could either confirm or reschedule their surgery, allowing other patients to be booked into unfilled slots.
One study in Norway found a statistically significant reduction in cancellation rates, as well as stabilization of cancellation rates and an increase in the number of surgeries performed (43). One Australian report indicated that cancellation rates decreased after the approach was implemented (78). No impact on wait times was provided.
Cancellation lists
Cancellation lists include names and contact details of patients willing to have surgery at short notice if a cancellation occurred, thereby reducing wait times by supporting full utilization of ORs. While this approach was mentioned both in the literature and interviews with respondents from Australia and Canada, no information on impact was found.
Flex days
Flex days referred to days in which ORs were made available for all services to use for urgent or emergent cases. This was done to help ensure that elective cases were not bumped. One interviewee from Canada suggested flex days have helped reduce cancellations of elective surgeries. No other information was found.
Innovative surgical approaches
As medical research continues to advance, innovative surgical approaches designed to improve OR efficiencies and outcomes have been introduced. Some innovative approaches have allowed patients to be discharged the same day as their surgery.
Examples from the literature and interviews include: SuperPATH, a new approach for hip replacement used in some Canadian provinces; one-day vascular surgery; and 23-hour appendectomies (79,80). Information about the impact of these surgical approaches was not found.
No-show policies
In the UK, patients have been penalized for missing scheduled surgeries without prior warning, except under exceptional circumstances. Specifically, patients returned to the back of the queue if they did not show up for treatment (81). No information on effectiveness was found.
Procedure rooms
Hospital rooms designated for small procedures that do not require an OR have been established in some centres. One respondent from Canada described the use of procedure rooms for suture removals and lumbar punctures which helped to increase capacity. No further information was found.
Pre-habilitation clinics
Pre-habilitation services are designed to optimize a patient’s overall health before they undergo elective surgery in order to ensure safer surgery, quicker recovery, and potentially reduce length of hospital stay. These services are commonly offered to patients undergoing orthopedic procedures, but have also been used for cardiothoracic, gynecology, and vascular surgeries. They may include education sessions, conditioning classes, and nutritional counselling depending on the targeted audience.
Based on findings from peer-reviewed studies, pre-habilitation programs were associated with reduced wait times for surgery and decreased length of stay; however, it was not possible to attribute either outcome to pre-habilitation programs, since they had been introduced alongside other approaches (40,42,46,49,80,82). One interview respondent suggested that pre-habilitation is costly and sometimes causes unnecessary delays in surgery.
Provider incentives
Providers who achieved pre-established targets have received financial or non-financial incentives. In 1996, in Spain, providers who managed to reduce the number of patients on the waiting list received bonuses in proportion to their salaries. Although the number of patients on the waiting list and mean waiting time decreased during this period, such incentives had been a part of a multipronged approach to reducing wait times (83,84). Non-financial incentives were identified in Canada, where surgeons received score cards comparing their performance to defined targets. One study found non-financial incentives alongside other approaches reduced wait times from referral to surgery (85).
Privately funded, privately delivered services
Several countries with publicly funded healthcare have a parallel private healthcare system, where patients can buy private insurance or pay out-of-pocket for privately delivered services. It has been suggested that parallel systems help to reduce wait times by allowing patients who can afford it to seek care in private facilities, while those who cannot are able to receive care in publicly funded facilities. One peer-reviewed study found that increased activity in the private healthcare system led to longer waits in Australia’s public healthcare system (86). Similarly, the grey literature did not demonstrate a positive impact of parallel private healthcare systems on wait times (87). No interview reported on the impact of the approach on wait times.
Prioritization of patients
Prioritization criteria have been used to identify surgical candidates and organize them on wait lists. Depending on the jurisdiction, they have considered: urgency or need alone; urgency and ability to benefit; or urgency and social/economic considerations, including ability to work, perform daily activities, and live independently, length of time waiting, and cost-effectiveness of the treatment. The development of these criteria has involved different groups (surgeons, family physicians, other health care providers, institutional administrators and patients) using different methods such as consensus, concept mapping, focus groups and Delphi panels. Criteria have been established for pediatric and adult surgery more broadly, and for specific procedures, including cataract surgery, cardiovascular surgery, and hip and knee replacement. In one case, health insurance has been used to create a priority ranking of patients (on sick leave) (88).
Regardless of the specific criteria, most examples from documents and interviews demonstrated that the use of criteria resulted in a reduction in wait times or in the number of patients waiting a specific amount of time (54,82,84,88,89). However, the extent to which other approaches implemented in addition to prioritization criteria contributed to the results was unclear.
The peer-reviewed literature also contained commentaries on some of the other benefits of prioritization. They primarily related to data collection and quality improvement. A uniform, standard way of prioritizing cases was seen as allowing for better benchmarking and leading to improved practices (90,91). The data collected for prioritization purposes had also facilitated comparisons across institutions and regions. It was felt that a prioritization approach increased consistency and fairness and ensured OR time was used with maximum effectiveness. In one case, it was noted that implementing the process brought to light previously undocumented issues, such as the simultaneous booking of both eyes for cataract surgery and variations in waiting time between surgeons (90).
At the same time, there have been concerns about how criteria are selected and weighted relative to one another. Classifying patients into broad categories for elective surgery wait lists has largely been subjective, and it was felt that clinicians can vary in their assessment of clinical and non-clinical factors in assigning a priority level.
Regular validation of wait lists
Waitlist validation involved the active review of waiting lists to ensure that all patients on the list still required surgery. Its purpose was to reassess patients’ clinical condition, update data and identify patients who were truly ready for care.
The literature reported that list validation reduced the number of patients on the waiting list, leading to reductions in wait times (50,92,93). However, according to one study, while the approach reduced wait times, the mean wait time still exceeded the recommended timeframe (50).
Subsidies for private health insurance or privately funded health insurance
Australia and Hong Kong provided patients with subsidies to encourage them to access privately funded, privately delivered surgeries in order to reduce strain on the public system. In Australia, the government began offering tax incentives in 1997 to encourage people to buy private health insurance after the percentage of the population covered by private health insurance fell from 50% to 30.5% between 1984 and 1998. This led to an increase in the percentage of both private health insurance coverage and the privately funded share of health care activity (84). In Hong Kong, the government implemented a public-private partnership program in which patients who chose to receive cataract surgery from a private ophthalmologist received a $5,000 subsidy to help offset the cost of the procedure (31). The program achieved the set target of 10,000 surgeries. While both programs were considered successful, impact on wait times were not reported.
Wait list management policies
Wait list management policies are designed to help clinics better manage their wait lists and accurately measure wait times. In one Canadian province, the management policy provide guidance around ongoing wait list maintenance and management (54). No evidence on the impact from the scoping review and interview was found.
Patient-targeted appropriateness initiatives
Patient-targeted appropriateness initiatives aim to help patients understand their options and choose the most appropriate treatment, reducing wait lists by ensuring only appropriate patients receive surgery. In two randomized-controlled trials in Canada, patients with osteoarthritis received education materials with information on treatment options and their benefits and harms. Both studies found no statistically significant difference in median total waiting times from screening consultation to a definitive decision (i.e., surgery or off wait list) between the groups receiving and not receiving the intervention (94,95). However, in one of the trials, patients exposed to the education materials obtained higher decision quality compared to the unexposed cohort (94). The second trial found no difference in decisions quality between groups (95). No further information was provided during interviews.
Ongoing monitoring, analysis, and reporting of wait times and other outcomes data
Ongoing monitoring involved continuous collection and monitoring of wait times, quality and safety data at local, regional or national levels. It was used to: identify barriers and opportunities for improvement; assess new initiatives designed to improve surgical access; and measure, monitor and manage surgical access.
According to documents and interviews, the approach was usually part of policies to reduce wait times (96-99). Ongoing monitoring was viewed as critical to the development of wait time measures, benchmarks and comparison across institutions and regions. While the effects of monitoring, alone, on wait times were unclear, the process was considered essential for addressing this issue.
Operations research and resources planning tools
Operations research refers to mathematical models applied to retrospectively analyze the impact of interventions on wait times and to explore possible effects of different scenarios on wait times. Availability of data through ongoing monitoring is a key component to building models.
Twelve studies, identified in the literature, developed models to analyze the effect of supply-side and demand-side approaches (100-111). Two studies developed models that were subsequently used to support strategic planning, redistribute OR capacity, make decisions around additional investments in infrastructure and staff, and revise eligibility criteria for surgery (104,110). During interviews, participants from Canada mentioned using hospital operations management tools as essential for capacity and resource planning.
Public reporting of wait times
Wait times have been made publicly available and regularly updated to increase transparency and accountability, document performance and reduce waiting times by allowing patients and physicians to make referral decisions based on such information. One Norwegian study found that wait times from referral to surgery were longer after public reporting was initiated (112). Several reports suggested few patients use information on waits to change surgeons or seek treatment in another hospital (83,84,112-114).
Wait time targets
Wait time targets or guarantees policies have been implemented in multiple countries with publicly funded healthcare systems. In theory, the policy guarantees patients receive surgery within a reasonable and clinically recommended timeframe. These policies may be legally or non-legally binding. Legally binding policies include: (I) those which specify legally binding wait time targets, enforced through positive or negative incentives; (II) those which specify legally binding wait time targets, have a mandatory offer of an alternative provider, and are enforced through positive or negative incentives; or (III) those which specify legally binding wait time targets, have a mandatory offer of an alternative provider, but do not indicate the use of enforcement mechanisms. Non-legally binding policies include: (I) those which specify non-binding targets with the offer of alternative provider or (II) those which specify non-binding targets.
A series of legally binding policies enforced using positive or negative incentives have been introduced in England (73,77,115-118). Several studies reporting on the impact of such policies found that while they reduced wait times 2 (77,116,119,120) and overall wait times (73,121-123), they also received criticism from healthcare professionals who felt they undermined professional autonomy, reduced staff morale, distorted clinical priorities (124), and manipulated signs of waiting lists (73,121-123).
In Norway, in the 1990s, a legally binding wait time guarantee was given to patients with “needs”, and by law, it had to offer treatment to patients at another provider if the guarantee was not fulfilled. However, the number of patients on the wait list and waiting more than 6 months increased. Consequently, the policy changed in 2004. After that, an assessment by a specialist had to take place within 30 days of referral, and if the patient met the requirements, she/he was given an individual maximum waiting time until start of treatment. The policy demonstrated little effect on mean waiting times from referral to surgery, but from 2006 to 2011, there was a reduction in the number of patients being given a maximum waiting time guarantee (125).
In 1992, Sweden instituted a non-legally binding guarantee for 12 procedures. Additional funding was provided. Three peer-reviewed studies and 2 reports in the grey literature concluded that there was a temporary reduction in wait times, which stopped when no new funds were provided (77,126-129). In 2005, a new policy for all elective surgeries was enacted, in which patients could choose another provider (public or private) if the guarantee was not fulfilled at the expense of the region where they resided. However, the policy had limited effect on wait times, with many patients uninformed about their rights to choose another provider (77,130). This led to a policy change in 2010 that introduced economic incentives to Health Authorities achieving wait time targets. One study compared overall wait times in Sweden to those in Norway, where such incentives had not been implemented, and found that they were lower in Sweden (131).
In Scotland, a non-legally binding wait time guarantee and an offer of an alternative provider were instituted in 2003. Mean wait times decreased after the policy was introduced (105,132). However, analyses also showed that low priority patients experienced a reduction in wait times at the cost of high-priority patients, whose wait times did not change over time. In 2011, Scotland implemented legally binding targets, but no information on the impact of the policy was found.
In Denmark, a non-legally binding wait time guarantee had no effect on wait times (77,133). Consequently, a new policy was introduced, in which patients were offered the option of another provider if the guarantee was not met. Additional funding was provided. While wait times declined, the percentage of patients seeking private hospitals increased during the same period (77).
In Canada, the federal government offered extra funding to provinces that committed publicly to establishing wait time guarantees for at least one procedure. In the first 5 years, most provinces had made progress in reducing wait times. However, the impact of the target times has not been consistent over time or across the country (134-136).
Overall, we identified 8 approaches with consistent positive evidence of effectiveness, listed in order of the number of sources of information which we reviewed:
- Targeted funding (60);
- Publicly funded, privately delivered services (48);
- Prioritization of patients (47);
- Same-day surgery and discharge (18);
- Streamlined pre-admission processes (18);
- Expanded roles for non-physicians (16);
- Standardized treatment pathways (16);
- Process improvement methodology (15);
- Regular validation of wait lists (7).
Six approaches were identified as having limited but promising evidence of effectiveness:
- Patient choice (36);
- Centralization of elective surgeries (14);
- Centralized surgical scheduling (14);
- Efficient use of ORs (9);
- Fast-track programs (4);
- Family doctors-led surgeries (3).
Two approaches were identified as having consistent negative evidence of effectiveness and none of the other strategies evaluated had enough information to determine their impact.
Discussion
This study included 366 different information sources describing 33 approaches with varying degrees of effectiveness in reducing wait times 2. Most were supply-side approaches, with 15 showing consistent or limited but promising positive impact.
The most effective policies were those comprising multiple supply and demand strategies targeting the whole patient pathway. They required collaboration between policymakers and healthcare providers, investment and even regulation changes.
Limitations
The intent of the review was to identify the range of approaches used in Canada and internationally to address wait times. Therefore, the search strategy did not include terms for specific approaches. As a result, it is possible that some studies of the effectiveness of specific approaches may have been missed. Those interested in implementing one or more of the approaches identified in this review may need to conduct a more in-depth systematic review to assess their effectiveness. This would involve critically appraising studies, selecting and synthesizing outcomes of interest, including patient and provider experience, length of stay, and emergency room (ER) readmissions. Strength of evidence criteria used in this review defined a positive effect as a documented reduction in any wait time metric (mean, median, number of patients on the waitlist). Third, the quality assessment relied on the amount of evidence available, regardless of type (grey or peer-reviewed study). Fourth, the research team used Google as one of the search engines. Currently, there are no guidelines on how to use this search engine in such reviews (137,138). Finally, the study was limited to English and French.
Conclusions
This study identified eight different strategies with consistent positive evidence of effectiveness in reducing the wait time for elective surgeries and an additional six strategies with more limited but promising evidence of effectiveness. The approaches reviewed reduced referral times by affecting supply, demand, or both.
Acknowledgments
Funding: This work was supported by a financial contribution from the Government of Alberta (No. 008560). The views expressed herein do not necessarily represent the official policy of the Government of Alberta. The Health Technology & Policy Unit, School of Public Health, University of Alberta receives a multiyear unrestricted grant from Alberta Health to conduct health evidence reviews to inform policy decisions in the province.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-96/coif). MEB reports that she is a recipient of academic grants from government and non-profit agencies. She receives honoraria from academic institutions for speaking engagements and is member of the ERAS Society Executive (non-profit). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- OECD. Waiting Times for Health Services. Paris: OECD Publishing, 2020.
- Alberta Health Services. Leading access transformation: Path to care. Alberta, Canada: Alberta Health Services, 2019.
- Health Quality Ontario. System Performance Ontario, Canada. 2021. Available online: https://www.hqontario.ca/System-Performance/Wait-Times-for-Surgeries-and-Procedures
- OECD. Health at a Glance 2017: OECD Indicators. Paris, France: OECD Publishing, 2017.
- Schneider EC, Sarnak DO, Squires D, et al. Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care. New York, USA: The Commonwealth Fund, 2017.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8:19-32. [Crossref]
- Kreindler SA. Policy strategies to reduce waits for elective care: a synthesis of international evidence. Br Med Bull 2010;95:7-32. [Crossref] [PubMed]
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169:467-73. [Crossref] [PubMed]
- Shetty A, Manimaran N, Reece-Smith H. Direct access day-case hernia surgery: A logical option for reduction in waiting time. Ambul Surg 2004;11:41-3. [Crossref]
- Downey M. Transformative cardiac care model streamlines procedures and reduces wait times. Ottawa (ON), Canada: Canadian Foundation for Healthcare Improvement, 2014.
- Ghai S, Lee SY, Bret PM, et al. Thyroid Biopsy Specialists: A Quality Initiative to Reduce Wait Times and Improve Adequacy Rates. Radiology 2015;276:894-9. [Crossref] [PubMed]
- Newey M, Clarke M, Green T, et al. Nurse-led management of carpal tunnel syndrome: an audit of outcomes and impact on waiting times. Ann R Coll Surg Engl 2006;88:399-401. [Crossref] [PubMed]
- Scottish Government. The Modern Outpatient: A Collaborative Approach 2017-2020. Edinburgh, Scotland: Scottish Government, 2017.
- Godsell G. A nurse-surgical post cuts waiting times and extends nurses' skills base. Prof Nurse 2004;19:453-5. [PubMed]
- Valsangkar NP, Eppstein AC, Lawson RA, et al. Effect of Lean Processes on Surgical Wait Times and Efficiency in a Tertiary Care Veterans Affairs Medical Center. JAMA Surg 2017;152:42-7. [Crossref] [PubMed]
- Brown R, Grehan P, Brennan M, et al. Using Lean Six Sigma to improve rates of day of surgery admission in a national thoracic surgery department. Int J Qual Health Care 2019;31:14-21. [Crossref] [PubMed]
- Kullar P, Harris F, Lloyd SK, et al. The use of Lean Thinking techniques in implementing the Department of Health, UK, 18-week waiting time directive for cochlear implantation. Cochlear Implants Int 2010;11:133-45. [PubMed]
- Interior Health. Interior Health Capital Strategy 2013-2023. British Columbia, 2013.
- Sullivan Healthcare Consulting Canada Co. Surgical services review and future state modeling. London (ON), Canada: Sullivan Healthcare Consulting Canada Co., 2012.
- Central Queensland Hospital and Health Service. 2014-2015 Annual Report. Rockhampton, Queensland: Central Queensland Hospital and Health Service, 2015.
- Adams R, Warner P, Hubbard B, et al. Decreasing turnaround time between general surgery cases: a six sigma initiative. J Nurs Adm 2004;34:140-8. [Crossref] [PubMed]
- Alberta Health Services. Alberta Health Services Annual Report 2012-2013. Alberta, Canada: Alberta Health Services Board, 2013.
- Alberta Health Services. Alberta Health Services Health Plan & Business Plan 2016-17. Alberta, Canada: Alberta Health Services Board, 2016.
- Grindle T. Efficiency initiative reduces wait times by half. Alberta: Alberta Health Services, 2013.
- Improving the quality of surgical care across Alberta [press release]. Alberta: Alberta Health Services, 2018.
- Initiative helps Edmonton hip, knee clinic reduce wait times [press release]. Alberta, Canada: Alberta Health Services, 2013.
- Kent H. Private contractors to reduce surgical waits at BC hospital. CMAJ 2003;169:328.
- MacKinnon JC. Wait times in Canada. Healthc Manage Forum 2017;30:190-2. [Crossref] [PubMed]
- Kirkwood G, Pollock AM. Patient choice and private provision decreased public provision and increased inequalities in Scotland: a case study of elective hip arthroplasty. J Public Health (Oxf) 2017;39:593-600. [PubMed]
- Alberta Health Services. Information for Surgical Contracts Facilities - Alberta Health Services Calgary Zone. Alberta: Alberta Health Services; 2019. Available online: https://www.albertahealthservices.ca/info/Page4896.aspx
- Hong Kong Hospital Authority. Cataract Surgeries Programme Hong Kong: Hong Kong Hospital Authority; 2019. Available online: https://www3.ha.org.hk/ppp/csp.aspx?lang=eng
- Queensland Government. Torres and Cape Hospital and Health Service. Newsletter - new ENT Project Manager. Queensland Government, 2017.
- Cour des comptes. L'avenir de l'assurance maladie. France: Cour des comptes, 2017.
- Palley HA, Pomey MP, Forest PG. Examining private and public provision in Canada's provincial health care systems: comparing Ontario and Quebec. International Political Science Review 2011;32:79-94. [Crossref]
- Cooper Z, Gibbons S, Jones S, et al. Does Competition Improve Public Hospitals' Efficiency? Evidence from a Quasi-Experiment in the English National Health Service. CEP Discussion Papers dp1125, Centre for Economic Performance, LSE. 2012.
- Boisjoly H, Freeman EE, Djafari F, et al. Reducing wait time for cataract surgery: comparison of 2 historical cohorts of patients in Montreal. Can J Ophthalmol 2010;45:135-9. [Crossref] [PubMed]
- Major Initiative in Outpatient Surgery [press release]. Stockholm, Sweden: Karolinska University Hospital, 2016.
- New unit helps waiting times fall in Swansea [press release]. Wales, UK: Welsh Assembly Government, 2006.
- Stevenson J. Albertans waiting less time for hip and knee surgery. Alberta, Canada: Alberta Health Services, 2014.
- Alberta Bone & Joint Health Institute. Alberta Hip and Knee Replacement Pilot Project: Scientific Evaluation Report. Alberta, Canada, 2007.
- Alberta Bone & Joint Health Institute. Alberta Bone & Joint Health Institute Calgary (AB), Canada, 2019. Available online: https://albertaboneandjoint.com/
- Fraser Health hip and knee replacement program helps people get back in the swing of things [press release]. British Columbia, Canada: Fraser Health, 2018.
- Hovlid E, Bukve O, Haug K, et al. A new pathway for elective surgery to reduce cancellation rates. BMC Health Serv Res 2012;12:154. [Crossref] [PubMed]
- Easto R, Shukla R, Rowland C, et al. Introducing paediatric grommet "rapid turnover" lists. A Quality Improvement Project. BMJ Qual Improv Rep 2016;5:eu210715. [Crossref] [PubMed]
- Ellis G, Spiers M, Coutts S, et al. Preoperative assessment in the elderly: evaluation of a new clinical service. Scott Med J 2012;57:212-6. [Crossref] [PubMed]
- Ministry of Health. Improving the System: Meeting the Challenge - Improving patient flow for electives. Wellington, New Zealand: Ministry of Health, 2012.
- Central Adelaide Local Health Network. Central Adelaide Local Health Network Annual Report 2014-15. Adelaide (SA), Australia: Government of South Australia, 2015.
- Wide Bay Hospital and Health Service. The Wide Bay Wave. Queensland Government: Wide Bay Hospital and Health Service, 2018.
- Williams DH, Iker C, Leith L, et al. Improving surgical access: the Vancouver experience. Can J Surg 2011;54:277-1. [Crossref] [PubMed]
- Briggs RJ, Smith KM, Dejager EM, et al. The active management of surgical waiting lists: a urological surgery case study. Aust Health Rev 2011;35:399-403. [Crossref] [PubMed]
- Sobolev BG, Fradet G, Kuramoto L, et al. Evaluation of supply-side initiatives to improve access to coronary bypass surgery. BMC Health Serv Res 2012;12:311. [Crossref] [PubMed]
- Nova Scotia Health Authority. Hip and Knee Action Plan. Nova Scotia, Canada: Nova Scotia Health Authority, 2018.
- Elective surgery queues getting shorter [press release]. Australia: Australian Associated Press, 2010.
- Alberta Health Services. Alberta Health Services Performance Report Q2 2011/12. Alberta, Canada: Alberta Health Services, 2011.
- Head L, Nessim C, Usher Boyd K. Innovative practice model to optimize resource utilization and improve access to care for high-risk and BRCA+ patients. Can J Surg 2017;60:37-44. [Crossref] [PubMed]
- Central Local Health Integration Network (LHIN). A Vision for ophthalmology services in Central LHIN Ontario. Central LHIN; 2019.
- Lewis R, Appleby J. Can the English NHS meet the 18-week waiting list target? J R Soc Med 2006;99:10-3. [Crossref] [PubMed]
- das McMurtry N. Backgrounder: Surgical wait times for publicly funded health services in Canada. Canada: Evidence Network, 2019.
- Friedman DM, Sokal SM, Chang Y, et al. Increasing operating room efficiency through parallel processing. Ann Surg 2006;243:10-4. [Crossref] [PubMed]
- Queensland Health. Operating Theatre Efficiency Guideline. Brisbane, Queensland: State of Queensland (Queensland Health), 2017.
- Cognetti DM, Nussenbaum B, Brenner MJ, et al. Current State of Overlapping, Concurrent, and Multiple-Room Surgery in Otolaryngology: A National Survey. Otolaryngol Head Neck Surg 2017;157:998-1004. [Crossref] [PubMed]
- Padegimas EM, Hendy BA, Lawrence C, et al. An analysis of surgical and nonsurgical operating room times in high-volume shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:1058-63. [Crossref] [PubMed]
- Usher S, Roberts C, Hughes K. Operating room efficiency. Montreal (QC), Canada: Health Innovation Forum, 2019.
- Guzmán Laura KP, Bolíbar Ribas I, Alepuz MT, et al. Impact on patient care time and tumor stage of a program for fast diagnostic and treatment of colorectal cancer. Rev Esp Enferm Dig 2011;103:13-9. [Crossref] [PubMed]
- Sorensen JR, Johansen J, Gano L, et al. A "package solution" fast track program can reduce the diagnostic waiting time in head and neck cancer. Eur Arch Otorhinolaryngol 2014;271:1163-70. [Crossref] [PubMed]
- Sanz-Santos J, Andreo F, Sánchez D, et al. Usefulness of a lung cancer rapid diagnosis specialist clinic. Contribution of ultrasound bronchoscopy. Arch Bronconeumol 2010;46:640-5. [Crossref] [PubMed]
- Macleod AM, Gollish J, Kennedy D, et al. Toward a joint health and disease management program. Toronto hospitals partner to provide system leadership. Healthc Q 2009;12:56-65. [Crossref] [PubMed]
- Gaynor M, Propper C, Seiler S. Free to Choose? Reform and Demand Response in the English National Health Service. National Bureau of Economic Research, 2012.
- Braadland Rustoen S, Storbraten A. Institutionalizing Lean in a Norwegian Public Hospital: The same-day surgery process at SI Lillehammer. Norwegian University of Science and Technology, 2017.
- Pioneering mobile heart clinic to help cut waiting times for North Wales patients [press release]. Wales, United Kingdom: NHS Wales, 2016.
- Blick G, Davies P, Esplin J. Review of mobile surgical services and related services. Australia: Sapere Research Group Limited, 2014.
- Ferris JD. Independent sector treatment centres (ISTCS): early experience from an ophthalmology perspective. Eye (Lond) 2005;19:1090-8. [Crossref] [PubMed]
- Propper C, Wilson D, Burgess S. Extending choice in English health care: The implications of the economic evidence. Journal of Social Policy 2006;35:537-57. [Crossref]
- Redaniel MT, Ridd M, Martin RM, et al. Rapid diagnostic pathways for suspected colorectal cancer: views of primary and secondary care clinicians on challenges and their potential solutions. BMJ Open 2015;5:e008577. [Crossref] [PubMed]
- Expert Panel for Patient-Based Funding. Better Access to Surgery, an expanded activity-based funding program. Québec: Gouvernement du Québec, 2014.
- Street A. Introducing activity-based financing: a review of experience in Australia, Denmark, Norway and Sweden. York, UK: Centre for Health Economics, University of York, 2007.
- Siciliani L, Borowitz M, Moran V. Waiting Time Policies in the Health Sector: What Works? Paris, France: OECD Publishing, 2013.
- New South Wales Government. March 2017 Surgery Newsletter New South Wales, Australia. NSW Government; 2017. Available online: https://www.health.nsw.gov.au/Performance/Pages/surgerynews-2017-03.aspx
- Surgery Strategic Clinical Network. Evidence Decision Support Program (EDSP). Edmonton (AB), Canada: Alberta Health Services, 2019. Available online: https://www.albertahealthservices.ca/scns/edsp.aspx
- Fraser Health. Hip and Knee Arthroplasty - Central Intake and Optimization Clinic Fraser Health Authority: Fraser Health Authority, 2019. Available online: https://www.fraserhealth.ca/Service-Directory/Services/Surgical-Services/hip-and-knee-arthroplasty---central-intake-and-optimization-clinic#.XLeAfTBKjRZ
- Scottish Executive. Fair to All, Personal to Each: The next steps for NHSScotland. Edinburgh, Scotland: Scottish Executive, 2004.
- Doerr CR, Graves SE, Mercer GE, et al. Implementation of a quality care management system for patients with arthritis of the hip and knee. Aust Health Rev 2013;37:88-92. [Crossref] [PubMed]
- Standing Committee of the Hospitals of the E. U. Waiting Lists and Waiting Times in Health Care- Managing Demand and Supply. Leuven, Belgium, 2001.
- Siciliani L, Hurst J. Tackling excessive waiting times for elective surgery: a comparative analysis of policies in 12 OECD countries. Health Policy 2005;72:201-15. [Crossref] [PubMed]
- Werle J, Dobbelsteyn L, Feasel AL, et al. A study of the effectiveness of performance-focused methodology for improved outcomes in Alberta public healthcare. Healthc Manage Forum 2010;23:169-74. [Crossref] [PubMed]
- Duckett SJ. Private care and public waiting. Aust Health Rev 2005;29:87-93. [Crossref] [PubMed]
- Canadian Health Services Research Foundation. A parallel private system would reduce waiting times in the public system. J Health Serv Res Policy 2006;11:253-4. [Crossref] [PubMed]
- Aakvik A, Holmås TH, Kjerstad E. Prioritization and the elusive effect on welfare - a Norwegian health care reform revisited. Soc Sci Med 2015;128:290-300. [Crossref] [PubMed]
- Curtis AJ, Russell CO, Stoelwinder JU, et al. Waiting lists and elective surgery: ordering the queue. Med J Aust 2010;192:217-20. [Crossref] [PubMed]
- Bellan L, Mathen M. The Manitoba Cataract Waiting List Program. CMAJ 2001;164:1177-80. [PubMed]
- Pomey MP, Martin E, Forest PG. Waiting List Management in Quebec: Implementing a System to Manage Access to Care. Kingston, Ontario: Queen's University, 2005.
- New South Wales Department of Health. NSW Department of Health Annual Report 2005/06. New South Wales, Australia: NSW Department of Health, 2006.
- New South Wales Department of Health. NSW Department of Health Annual Report 04/05. North Sydney, NSW: NSW Department of Health, 2005.
- Stacey D, Hawker G, Dervin G, et al. Decision aid for patients considering total knee arthroplasty with preference report for surgeons: a pilot randomized controlled trial. BMC Musculoskeletal Disorders 2014;15:54. [Crossref] [PubMed]
- Stacey D, Taljaard M, Dervin G, et al. Impact of patient decision aids on appropriate and timely access to hip or knee arthroplasty for osteoarthritis: a randomized controlled trial. Osteoarthritis Cartilage 2016;24:99-107. [Crossref] [PubMed]
- Department for Health and Ageing. Department for Health and Ageing Annual Report 2012-13. Adelaide, SA: Department for Health and Ageing, Government of South Australia, 2013.
- Alberta Health Services. Wait Time Measurement, Management, and Reporting of Scheduled Health Services Procedure Manual. Alberta: Alberta Health Services, 2013.
- BC Surgical Patient Registry. Victoria (BC), Canada: Provincial Health Services Authority; 2019. Available online: http://www.phsa.ca/our-services/programs-services/bc-surgical-patient-registry
- Wait Time Data Collection. British Columbia, Canada: Government of British Columbia; 2019. Available online: https://www2.gov.bc.ca/gov/content/health/accessing-health-care/surgical-wait-times/understanding-wait-times/wait-time-data-collection
- Abásolo I, Barber P, González López-Valcárcel B, et al. Real waiting times for surgery. Proposal for an improved system for their management. Gac Sanit 2014;28:215-21. [Crossref] [PubMed]
- Akkerman R, Knip M. Reallocation of beds to reduce waiting time for cardiac surgery. Health Care Manag Sci 2004;7:119-26. [Crossref] [PubMed]
- Antelo M, Reyes Santias F, Martinez Calvo A. Bed Capacity and Surgical Waiting Lists: A Simulation Analysis. European Journal of Government and Economics 2015;4:118-33. [Crossref]
- Askildsen JE, Holmås TH, Kaarboe O. Prioritization and patients' rights: analysing the effect of a reform in the Norwegian hospital sector. Soc Sci Med 2010;70:199-208. [Crossref] [PubMed]
- Comas M, Castells X, Hoffmeister L, et al. Discrete-event simulation applied to analysis of waiting lists. Evaluation of a prioritization system for cataract surgery. Value Health 2008;11:1203-13. [Crossref] [PubMed]
- Januleviciute J, Askildsen JE, Kaarboe O, et al. The impact of different prioritisation policies on waiting times: case studies of Norway and Scotland. Soc Sci Med 2013;97:1-6. [Crossref] [PubMed]
- Kougias P, Tiwari V, Berger DH. Use of simulation to assess a statistically driven surgical scheduling system. J Surg Res 2016;201:306-12. [Crossref] [PubMed]
- Kumar A, Costa AM, Fackrell M, et al. A Sequential Stochastic Mixed Integer Programming Model for Tactical Master Surgery Scheduling. European Journal of Operational Research 2018;270:734-46. [Crossref]
- Persson M, Persson JA. Health economic modeling to support surgery management at a Swedish hospital. Omega-International Journal of Management Science 2009;37:853-63. [Crossref]
- Sperandio F, Gomes C, Borges J, et al. An Intelligent Decision Support System for the Operating Theater: A Case Study. IEEE Trans Autom Sci Eng 2014;11:265-73. [Crossref]
- Tako AA, Kotiadis K, Vasilakis C, et al. Improving patient waiting times: a simulation study of an obesity care service. BMJ Qual Saf 2014;23:373-81. [Crossref] [PubMed]
- Tuft S, Gallivan S. Computer modelling of a cataract waiting list. Br J Ophthalmol 2001;85:582-5. [Crossref] [PubMed]
- Kjerstad E, Kristiansen F. Working paper no. 21/05 Free choice, waiting time and length of stay in Norwegian hospitals. Bergen, Norway: Institute for Research in Economics and Business Administration, 2005.
- Rachlis MM. Public Solutions to Health Care Wait Lists. Canadian Centre for Policy Alternatives, 2005.
- Schut FT, Varkevisser M. Tackling hospital waiting times: the impact of past and current policies in the Netherlands. Health Policy 2013;113:127-33. [Crossref] [PubMed]
- Marques E, Noble S, Blom AW, et al. Disclosing total waiting times for joint replacement: evidence from the English NHS using linked HES data. Health Econ 2014;23:806-20. [Crossref] [PubMed]
- Appleby J, Boyle S, Devlin N, et al. Do English NHS waiting time targets distort treatment priorities in orthopaedic surgery? J Health Serv Res Policy 2005;10:167-72. [Crossref] [PubMed]
- Robinson D, Bell CM, Møller H, et al. Effect of the UK government's 2-week target on waiting times in women with breast cancer in southeast England. Br J Cancer 2003;89:492-6. [Crossref] [PubMed]
- Reddy S, Jones P, Shanthanna H, et al. A Systematic Review of the Impact of Healthcare Reforms on Access to Emergency Department and Elective Surgery Services: 1994-2014. Int J Health Serv 2018;48:81-105. [Crossref] [PubMed]
- Dimakou S, Parkin D, Devlin N, et al. Identifying the impact of government targets on waiting times in the NHS. Health Care Manag Sci 2009;12:1-10. [Crossref] [PubMed]
- Dawson D, Jacobs R, Martin S, et al. The Impact of Patient Choice and Waiting Time on the Demand for Health Care: Results from the London Patient Choice Project. Applied Economics 2006;38:1363-70. [Crossref]
- Propper C, Burgess S, Gossage D. Competition and Quality: Evidence from the NHS Internal Market 1991–9*. The Economic Journal. 2008;118:138-70. [Crossref]
- Propper C, Sutton M, Whitnall C, et al. Did 'targets and terror' reduce waiting times in England for hospital care? The B.E. Journal of Economic Analysis & Policy 2008; [Crossref]
- Propper C, Sutton M, Whitnall C, et al. Incentives and targets in hospital care: Evidence from a natural experiment. Journal of Public Economics. 2010;94:318-35. [Crossref]
- Mannion R, Davies H, Marshall M. Impact of star performance ratings in English acute hospital trusts. J Health Serv Res Policy 2005;10:18-24. [Crossref] [PubMed]
- Ringard Å, Sagan A, Sperre Saunes I, et al. Norway: health system review. Health Syst Transit 2013;15:1-162. [PubMed]
- Inglis T, Armour P, Inglis G, et al. Rationing of hip and knee referrals in the public hospital: the true unmet need. N Z Med J 2017;130:39-48. [PubMed]
- Hanning M. Maximum waiting-time guarantee--an attempt to reduce waiting lists in Sweden. Health Policy 1996;36:17-35. [Crossref] [PubMed]
- Hanning M, Lundström M. Waiting for cataract surgery--effects of a maximum waiting-time guarantee. J Health Serv Res Policy 2007;12:5-10. [Crossref] [PubMed]
- Rae D. Getting Better Value for Money from Sweden's Healthcare System. OECD Economics Department, 2005.
- Hanning M, Åhs A, Winblad U, et al. Impact of increased patient choice of providers in Sweden: cataract surgery. J Health Serv Res Policy 2012;17:101-5. [Crossref] [PubMed]
- Scandinavian Obesity Surgery Registry. SOReg 2016: Norway-Sweden first joint report. 2017.
- Bowers J. Waiting list behaviour and the consequences for NHS targets. J Oper Res Soc 2010;61:246-54. [Crossref]
- Pedersen KM, Christiansen T, Bech M. The Danish health care system: evolution--not revolution--in a decentralized system. Health Econ 2005;14:S41-57. [Crossref] [PubMed]
- Wait Time Alliance. Time to close the gap: report card on wait times in Canada. Wait Time Alliance, 2014.
- Wait Time Alliance. No more time to wait: Towards benchmarks and best practices in wait time management. Canada: Wait Time Alliance, 2005.
- Wait Time Alliance. It's about time! Achieving benchmarks and best practices in wait time management. Canada: Wait Time Alliance, 2005.
- Adams J, Hillier-Brown FC, Moore HJ, et al. Searching and synthesising 'grey literature' and 'grey information' in public health: critical reflections on three case studies. Syst Rev 2016;5:164. [Crossref] [PubMed]
- Mahood Q, Van Eerd D, Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods 2014;5:221-34. [Crossref] [PubMed]
Cite this article as: Stafinski T, Nagase FNI, Brindle ME, White J, Young A, Beesoon S, Cleary S, Menon D. Reducing wait times to surgery—an international review. J Hosp Manag Health Policy 2022;6:29.

