
Revitalizing the Italian NHS: remarks on the 2021–2026 national recovery plan (next generation EU)
Introduction
The first cases of coronavirus disease (COVID-19) were recorded in late 2019. By February 2020, the disease had begun to spread throughout Europe, where Italy was the first country to be hit by the pandemic. Overall, the country’s national health service is reputed to provide quality health services. Indeed, nearly all Italian residents are registered with the NHS, which covers most of the medical costs in hospitals and physician consultations (OECD 2019), and hospitals are described as providing high-quality treatment for patients requiring acute care. As Morciano and Caredda (1) state, “Italian prevention services are largely public and free at point of delivery. Immunisation and screening programmes represent priorities in the public health area, although with differences in services between regions”.
Yet there remain wider issues that hinder NHS performance. Italy has a decentralized healthcare system organized by region and a weak governance structure that generates inequalities, with poor national coordination between the country’s 20 regions (2). There is also the problem that the pandemic response plan appeared to be outdated when the crisis emerged (The Guardian, 13 August 2020 https://www.theguardian.com/world/2020/aug/13/italy-pandemic-plan-was-old-and-inadequate-covid-report-finds).
The infection rate rose rapidly after the first recorded case of COVID-19 (23 February 2020), with nearly 3,000 new infections and 100 deaths occurring in less than two weeks. The Italian government issued a Decree of the President of the Council of Ministers (DPCM) announcing a national lockdown shortly thereafter (11 March through 3 May 2020), followed suit by other European countries over the subsequent weeks. The pandemic had gone global, escaping the control of many countries. And it continues to spread by variants. Presently, the number of COVID-19 cases has begun to increase again in Italy, and localized lockdowns were issued between October 2020 and the first half of 2021. While the situation had stabilized during the second half of 2021, the emergence of the new omicron variant aroused renewed alarm in early 2022.
The pandemic has created numerous challenges for the Italian NHS. The national recovery plan will need to address several, among which the following are of particular importance.
Need for a stronger primary care network and more effective home care services
The initial waves of the pandemic soon showed that the resiliency of the NHS relied on the effectiveness of primary care services, tracing COVID-19 patients and treating them at home in an effort to relieve the burden on hospitals. As stated by Plagg et al. (3), Italy has neglected its primary healthcare system: there are only 89 general practitioners per 100,000 inhabitants, a rate far below that of Germany (167.4) and France (155.5). Lombardy, for instance, which disposes of abundant (medical) resources, has 6,143 general practitioners (74/100,000 inhabitants), 78% of which were over age 55 in 2019. The focus on hospitals early during the COVID-19 pandemic left primary care physicians in many regions without testing resources, adequate personal protection equipment (PPE), and network support. The lack of empowerment is mirrored in the pandemic’s mortality statistics. The pandemic revealed that a robust primary healthcare system, operating in cooperation between public and private healthcare facilities and supported by nursing staff could have effectively monitored many non-critically ill patients at home.
Shortage of healthcare professionals, capacity, and capability
Italy faced a shortage of health professionals during the COVID-19 pandemic (4). This occurrence signals a warning that adequate skills mix among healthcare workers is essential for ensuring sufficient delivery of health services, especially in a medical crisis. For example, Sprung et al. (5), in addressing the preparation of hospitals for an influenza pandemic or a mass disaster, underline how surge capacity for a hospital depends on the number of trained intensive care unit (ICU) staff. Health professionals were often under- or over-skilled for the tasks they had to perform during the medical crisis, leading to an inefficient deployment of human resources as a consequence.
Quality and availability of physical and material resources in healthcare
Physical and material resources are an essential component of a health system and factor into its performance and resilience. Indeed, they are crucial for the delivery of quality healthcare. During the height of the COVID-19 pandemic, there was a shortage of ICU beds. The Corriere della Sera, the most impactful Italian newspaper, reported a “historical shortage” in an article dated March 2020 (6). Another example was the lack of a consistent supply of PPE. Doctors Without Borders (11 April 2020) reported that health workers in many countries where they intervened routinely experienced “shortages of crucial items such as masks, aprons, and testing equipment.” (7). It is therefore relevant to consider material resources in an analysis of health system resilience (8).
Delay in technology innovation and renovation
What became quickly clear during the COVID-19 pandemic is that the NHS has to undertake major leaps forward in the adoption of modern technology to deliver its health services. Digitalization, telemedicine, and big data management are just a few areas where improvements need to be made. In addition, the crisis revealed the obsolescence of much of the technological assets (imaging, diagnostics, minor equipment, etc.). More than 60% of the assets in Italian hospitals are physically or technologically obsolete. An investment strategy is acutely needed (9).
Complex multisectoral collaboration and coordination
The World Health Organization (WHO) defines multisectoral preparedness coordination as “deliberate collaboration between stakeholders from multiple and diverse sectors and disciplines working towards the shared goal of enhanced health emergency preparedness” (10). As proof of the relevance of such coordination, the COVID-19 pandemic has had a major impact not only on the health systems of many countries but also on their socioeconomic and education systems. The United Nations reports that “the COVID-19 pandemic has created the largest disruption of education systems in history, affecting nearly 1.6 billion learners in more than 190 countries and all continents.” (11).
For example, the first lockdown in Italy (March 2020) kept students home from school for months. This has had two implications: the education sector has had to coordinate with the health sector for crisis containment through school non-attendance; the education sector has had to adapt to the emergency situation and develop alternative ways of teaching through distance learning. Another problematic aspect during the COVID-19 pandemic has been the use of public transport, signaling the need for coordination between the health sector and the Ministry of Public Transport. It was with these points in mind that the recovery plan was developed and approved by the Italian government. The following section illustrates its framework and content.
The next generation EU plan
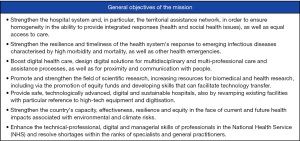
In spring 2021 the Next Generation EU plan was approved by the Italian Parliament and then by the EU Commission. The recovery and resiliency national plan—PNRR (the Italian acronym for the Next Generation EU plan) is composed of six lines of action, called Missions, of which healthcare is the sixth, with a total of €15,63 billion earmarked. The Mission is important because the pandemic has underscored the universal value of health and its nature as a fundamental public good. Many are the general objectives of the healthcare mission and they are clearly described in the document sent to the EU last spring (Figure 1) (12).
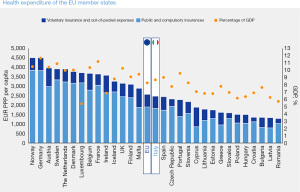
Another aim of the Plan is to improve Italy’s position in comparison to other EU countries on annual expenditures for the national healthcare sector (Figure 2) (13). The figure highlights the need of the NHS (in total expenditure and in relation to the percentage of GDP) for additional resources.
The Mission is divided into two lines of actions (Tables 1,2): one is focused on primary and intermediate care and telemedicine (M6C1) and the other on healthcare innovation, research, and innovation (M6C2). The specific focus of M6C1 is home care and chronic disease management. A major objective is to overcome the fragmentation and the structural gaps between the regional health systems by ensuring homogeneity in access to care and provision of essential care levels. The elderly and chronic patients can seek care from primary care services and their family doctors (general practitioners). The slogan of M6C1 is “Home is the first point of care”. The aim is to manage patients with type II diabetes, hypertension, and other conditions not requiring hospital admission (4 billion euros budgeted). The trade-off is not between primary and hospital care because M6C1 takes into account the importance of intermediate care and the needs of patients who do not need hospitalization but rather healthcare and surveillance that they could not receive otherwise at home (2 billion euros budgeted plus 1 billion euros more for setting up country hospitals).
Table 1
| 2021 | 2022 | 2023 | 2024–2026 | |
|---|---|---|---|---|
| M6-Healthcare | 0.1 | 0.1 | 0.2 | 0.3 |
| M6C1 (1st line of action) | 0.0 | 0.0 | 0.1 | 0.2 |
| M6C2 (2nd line of action) | 0.1 | 0.1 | 0.1 | 0.1 |
| Total of the six missions | 0.7 | 2.0 | 3.0 | 3.1 |
Source: Ministry of Economy and Finance PNRR pg. 258.
Table 2
| 2021 | 2022 | 2023 | 2024–2026 | |
|---|---|---|---|---|
| M6-Healthcare | 0.1 | 0.1 | 0.2 | 0.4 |
| M6C1 (1st line of action) | 0.0 | 0.0 | 0.1 | 0.1 |
| M6C2 (2nd line of action) | 0.1 | 0.1 | 0.1 | 0.3 |
| Total of the six missions | 0.7 | 2.2 | 3.5 | 4.0 |
Source: Ministry of Economy and Finance PNRR pg. 269.
The PNRR funds will be used to create community houses and country hospitals, so to reduce the pressure on large hospitals, while providing an alternative to home care for patients living on their own in cities or in rural areas or who cannot be treated at home for logistic reasons. The objective of M6C1 is to create and/or adapt 381 hospitals, by 2026.
M6C2 is the second line of action for the healthcare sector (8.62 billion euros budgeted). The two main reforms are: technological and digital upgrade (7.36 billion euros budgeted) and training and scientific research and technological transfer (1.26 billion euros budgeted). The first reform entails three main capital investments: upgrade of hospital technology and digital infrastructure (4.05 billion euros budgeted), new safe and sustainable hospitals (1.64 billion euros budgeted) and data (hard and software) management (1.67 billion euros budgeted). The second reform is about training, scientific research, and technological transfer. It entails two capital investments: empowerment of biomedical research (0.52 billion euros budgeted) and technical, professional, digital and managerial skills development of NHS personnel. The most relevant action is the link between the first investment and the first reform (upgrade of hospital technology and digital infrastructure), resulting in the purchase of new equipment (magnetic resonance systems, linear accelerators).
Like the population in general, so too the NHS personnel is aging. Investment No. 2 of the second reform (training in technical, professional, digital and managerial skills of NHS personnel) has allocated funds for 900 scholarships for the period 2021–2023 for young physicians interested in entering primary care who will replace the many general practitioners going into retirement. A total of 1.26 billion euros is budgeted to be awarded by mid 2026.
This is a brief description of the objectives and the resources budgeted by the National Plan for Recovery and Resiliency and funded by the European Union. But is the plan appropriate? Though the objectives are arguably the “right ones” for the future of the NHS and the decision making and the planning process was very well managed, there remain concerns about its implementation. From a managerial point of view, it is essential to have additional resources. While a huge amount of euros has been allocated, this is not sufficient. Given the inherent heterogeneity of the Italian NHS and its regional organization, the question arises about who will manage these additional recourses. Will they be managed centrally or locally? If managed centrally, their implementation will be more standardized and somehow less punctual, whereas if managed locally, the concern arises about the ability of the regions to spend the resources effectively (14).
Before describing the governance mechanism of this structural plan, it is important to mention the sheer amount of funds more than 15 billion euros for the healthcare sector, for a total of 191.5 billion euros for the six missions up to 235.6 billion euros if other programs are taken counted in (13.5 billion euros from React EU and 30.6 billion euros from the complementary fund). Two-thirds of the total amount of resources are to be returned to the EU.
The public administration will select experts to manage and monitor the projects, while the plan will be coordinated centrally by the Ministry of Economy and Finance. In addition, the President of the Council of Ministers (chief executive power) will be in charge of monitoring the process and the progress of the plan. An information system will be put in place to monitor achievement of the budgeted targets. The administration will periodically report to the Parliament and to the EU Commission.
The Next Generation EU will end in 2026. But what if a new pandemic breaks out? The lesson learnt is that not only does the NHS have to be prepared and operate quality health services but also greater effort should be undertaken to increase the health literacy of citizens. Understanding the importance and the effectiveness of vaccines is vital in this context, where too many issues have been raised by people who are hesitant or refuse to get vaccinated for all sorts of reasons they strongly believe in.
Conclusions
The Next Generation EU plan approved by the Italian government includes specific measures that could greatly benefit the Italian NHS. As significant funds are dedicated to improvements in technology and facilities, the plan provides the resources that could ultimately—after over a decade of efforts to put the NHS under financial scrutiny—provide the much needed resources to improve (or restore to an acceptable level) the assets of the healthcare system.
Yet, while some hope that this will mark the starting point of a longer and larger process of investment in the NHS, others are skeptical about administrative capacity and capability for implementation. Furthermore, there remains the issue of sustainability, as the incoming funds are earmarked for building and renovating assets, which then will require staff to operate and manage them. Nowhere in sight is there a complementary plan on how to finance the increase in annual NHS expenditures for staffing the community hospitals and houses (primary care centers). Finally, the time frame for the recovery plan actions seems relatively short compared to the investments managed by the NHS in the past, which were often complicated and delayed by red tape.
Hence, one can say that the prospects for the NHS remain uncertain and that implementation of the recovery plan (Next Generation EU plan) poses a puzzle. Nonetheless, we now dispose of resources for the health system which were unexpected two years ago (albeit much needed). Their implementation could constitute a stress test for the NHS to improve its capability and to reduce red tape and develop a more effective managerial culture and mindset.
Acknowledgments
Funding: None.
Footnote
Provenance and peer review: This article was commissioned by the Guest Editors (Stephen J. O’Connor, Nancy Borkowski and Katherine A. Meese) for the series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences” published in Journal of Hospital Management and Health Policy. The article has undergone external peer review.
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-78/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-78/coif). The series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Morciano L, Caredda E. The Governance of Prevention in Italy. Biomedicine & Prevention Issues 2018;3:173.
- Mauro M, Maresso A, Guglielmo A. Health decentralization at a dead-end: towards new recovery plans for Italian hospitals. Health Policy 2017;121:582-7. [Crossref] [PubMed]
- Plagg B, Piccoliori G, Oschmann J, et al. Primary Health Care and Hospital Management During COVID-19: Lessons from Lombardy. Risk Manag Healthc Policy 2021;14:3987-92. [Crossref] [PubMed]
- Sanfelici M. The Italian Response to the COVID-19 Crisis: Lessons Learned and Future Direction in Social Development. The International Journal of Community and Social Development 2020;2:191-210. [Crossref]
- Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine's Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med 2010;36:428-43. [Crossref] [PubMed]
- Corriere Della Sera. Le terapie intensive ormai al limite «Presto più dimessi che nuovi arrivi». Available online: https://www.corriere.it/cronache/20_marzo_30/terapie-intensive-ormai-limitepresto-piu-dimessi-che-nuovi-arrivi-773bd9e0-72b6-11ea-bc49-338bb9c7b205.shtml
- Doctorswithoutborders.org. Doctors Without Borders. Available online: https://www.doctorswithoutborders.org/what-we-do/news-stories/news/covid-19-crisis-update-racing-respond-pandemic-over-70-countries
- Mazzucato M, Kattel R. COVID-19 and public-sector capacity Oxf Rev Econ Policy 2020;36:S256-69. [Crossref]
- Petracca F, Ciani O, Cucciniello M, et al. Harnessing Digital Health Technologies During and After the COVID-19 Pandemic: Context Matters. J Med Internet Res 2020;22:e21815. [Crossref] [PubMed]
- World Health Organization 2020. Multisectoral Preparedness Coordination Framework: best practices, case studies and key elements of advancing multisectoral coordination for health emergency preparedness and health security. Available online: https://apps.who.int/iris/handle/10665/332220
- United Nations 2020. Policy Brief. Education during COVID 19 and beyond. Available online: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf
- Italian Ministry of Economics and Finance. The Recovery and Resilience Plan: Next Generation Italia. Available online: https://www.mef.gov.it/en/focus/documents/PNRR-NEXT-GENERATION-ITALIA_ENG_09022021.pdf
- Italian Ministry of Economics and Finance. The Next generation Italia (revised version). Available online: https://italiadomani.gov.it/it/home.html
- Rodríguez-Pose A, Garcilazo E. Quality of government and the returns of investment: Examining the impact of cohesion expenditure in European regions. Reg Stud 2015;49:1274-90. [Crossref]
Cite this article as: Vendramini EA, Lega F. Revitalizing the Italian NHS: remarks on the 2021–2026 national recovery plan (next generation EU). J Hosp Manag Health Policy 2022;6:30.

