
Accountable care team membership and distress: is accountable care team membership associated with lower distress during a crisis?
Introduction
Interprofessional collaboration remains at the forefront of both research and clinical problem solving, as healthcare organizations seek ways to provide high-quality patient care in the modern value-based healthcare environment. Interprofessional collaboration occurs “when multiple health workers from different professional backgrounds work together with patients, families, caregivers and communities to deliver the highest quality of care” (1). In its ideal form, interprofessional collaboration provides a synergistic relationship between professionals who communicate effectively and align around common goals related to patient care (2).
Over time, the modern healthcare environment has challenged the traditional hierarchical healthcare team to adopt a more flattened and collaborative model for shared decision making (3). While care teams are working toward more collaborative decision making, a similar trend exists at the organizational level, as front-line staff are becoming increasingly involved in problem solving for systemic organizational issues (4).
In recent years, few hospitals have begun to formally develop and implement structures and processes to further promote interprofessional collaboration and leadership at the microsystem level (e.g., unit, service) with the goal to improve care quality, efficiency, and patient and provider experience (2,5,6). Termed by some as the Accountable Care Team (ACT) model, recent publications have described common core components that define an ACT. These include: (I) designated unit-based leaders, typically a physician-nurse manager leadership dyad, (II) cohorting of patients, physicians and team members to the unit as much as possible, (III) high-performing daily interprofessional team care planning rounds, (IV) proactive leadership dyad assessment of patient experience, and (V) access to unit-level data for use by the team in performance improvement (Table 1) (2,5). Early results demonstrate this ACT model of care improves both interprofessional collaboration and horizontal problem solving on the frontlines of patient care (2,5). This is demonstrated by outcomes including but not limited to decreased average length of stay and case-mix index adjusted variable direct costs on inpatient units, reduced turnover times and increased revenue in the operating room setting, and improved engagement and job satisfaction across disciplines in both settings (2,5).
Table 1
| UABHS ACT core components | Description |
|---|---|
| Leadership Triad | Identification of the physician and operational personnel who will serve as the ACT leaders. The nursing role is typically filled by the unit nurse managers. This leadership triad is responsible for leading a broader interprofessional ACT problem-solving team |
| Interprofessional ACT problem-solving team | Identification of the broader ACT that includes one to two representatives from the other disciplines caring for patients on the unit (typically acute rehab therapists, care transitions staff, and pharmacists) |
| Cohorting | Cohorting of patients, physicians and team members to the unit as much as possible; this requires higher system-level support, thus connecting the microsystem to the macrosystem |
| Leadership Development Training | Delivered to the leadership triad members either preceding or following the problem-solving curriculum |
| Systems Thinking Curriculum & Simple Problem-Solving Training | Delivered to the larger ACT leadership team either preceding or following the leadership development curriculum by the CPT team |
| Access to unit-level data | Included in the problem-solving training is access and teaching teams in the use of the ACT dashboard that contains relevant unit/service level for use by the team in performance improvement |
| Interprofessional ACT team weekly problem-solving meetings | Following completion of the problem-solving training, the broader ACT team conducts weekly meetings in which they utilize skills learned to conduct process improvement for their microsystem, guided by data provided and organizational priorities |
| Daily Interprofessional Rounds | High-performing daily interprofessional team TOC rounds, as measured by a TOC quality assurance assessment tool developed and administered by the Care Transitions Department |
| Proactive assessment of patient experience | ACT teams, typically members of the leadership triad, develop process for proactive assessment and inclusion of the patient/family experience in performance improvement |
ACT, Accountable Care Team; CPT, Clinical Practice Transformation; TOC, Transition of Care.
Simultaneous to the need to improve care quality and efficiency, healthcare organizations are also becoming increasingly concerned with employee wellbeing, as workforce demands, and clinician burnout have risen significantly in the past decade (7). The American Hospital Association identifies burnout of healthcare professionals as a major threat to the healthcare industry, due to its association with medical errors and financial loss (8). Preliminary research has shown an increase in provider burnout associated with the COVID-19 pandemic, thus making employee wellbeing increasingly relevant to the current healthcare landscape (9). The Institute for Healthcare Improvement has suggested the importance of “psychological personal protective equipment (PPE)” in protecting healthcare workers during a crisis (10). The purpose of this paper is to understand whether ACT membership was associated with lower distress during a major crisis, particularly the COVID-19 pandemic. As the intervention seeks to improve a sense of community and belonging, as well as improved autonomy, we propose the following hypothesis:
H1. Healthcare workers who are ACT members will exhibit lower distress during COVID-19, compared to their peers who are not ACT members. We present the following article in accordance with the SURGE reporting checklist (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-70/rc).
Methods
Study design
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the University of Alabama at Birmingham (No: IRB-300005398) and informed consent was taken from all of the participants. In June-July 2020, an optional online employee survey was sent to 6,276 medical center employees by the UAB Medicine Office of Wellness. Invitation emails exhorting potential participants were sent in a three-week window. To take part in our survey, respondent had to choose one of the following roles: clinician, clinical support staff, nurse, advanced practice provider (APP), and non-clinical support staff. Participants were not compensated after completing the survey. The survey measured levels of distress, resilience, and individual and organizational-level factors. In addition, respondents were asked to identify major work, clinical and non-work stressors. In this time frame there were nine ACTs in various stages of development: four receiving leadership development training and five had completed or were actively receiving training in systems-based problem solving from the Clinical Practice Transformation (CPT) department. Also, in this time frame the hospital had two existing non-ICU COVID-19 units and a third COVID-19 unit to start in July 2020, all of which were ACT units.
ACT intervention plan
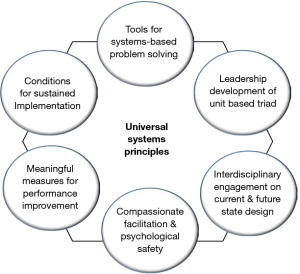
At the University of Alabama (UAB) Hospital, we defined the core components and implementation plan to develop ACTs on our acute care units using strategies from published ACT manuscripts as well as phone consultations with other institutions with active ACTs. Using this information, we included several additional components to the ACT development process for our organization (Table 1). These additions include the formation of a leadership triad for each new ACT team that consists of a physician, nursing, and operational/managerial lead. This leadership triad is responsible for leading a broader ACT leadership team that also includes one to two representatives from the other disciplines caring for patients on the unit (typically acute rehab therapists, care transitions staff, and pharmacists). Another key addition to our ACT development strategy is the creation of a leadership curriculum delivered to the triad, and problem-solving curriculum that is delivered over a series of sessions to the broader ACT leadership team. The goal of this formalized training is to equip and empower each ACT to independently lead performance improvement at the microsystem level in a disciplined manner, resulting in sustained change and improvement. The leadership curriculum was developed and delivered by Leadership Development Office (LDO) faculty to the triad members and skills taught included leadership and team principles, performance management, relationships and communication, and productivity/meeting management proficiencies. The problem-solving training is delivered by a team from the hospital’s CPT Department. CPT developed the curriculum based on an integration of universal systems principles, frontline interdisciplinary engagement, and peer support principles, see Figure 1. The CPT team facilitates problem solving in high impact areas during their engagement to ultimately equip front-line ACT members with skills and tools for sustained problem-solving. An ACT Implementation Oversight team began implementing ACTs at the unit level in February of 2019 and is currently engaged in a comprehensive plan to rollout ACTs across 32 units.
Dependent variable
Distress levels were measured by the validated 9-item Well-Being Index (WBI) measurement tool (11-14). The WBI results in scores ranging from −2 to 9, with higher scores indicating higher distress. In the general population, a WBI ≥2 is considered “high distress.” Higher WBI distress scores have been correlated to a number of detrimental outcomes such as an increased risk of burnout, medical error, poor quality of life and suicidal ideation (13,15,16).
Independent variables
Based on prior research, in which we explore distress among health care workers during the summer of 2020, we incorporated predictors that were significantly associated with wellbeing (17). In the following section we will discuss the structure and operationalization of all independent variables included in our analysis.
Work-related factors
Respondents were asked to identify their role and work-related factors such as location, clinical specialty, exposure to aerosolizing procedures, shift types, and ACT membership status.
Moral distress was measured using a single-item measure from the 2018 annual Veteran’s Affairs (VA) employee survey (18), asking how frequently they experienced moral distress such as feeling like they could not do the right thing, or were unsure of what the right thing to do was (5 point scale, with 5 indicating almost every work day).
Perceived organizational support was measured using a 3-question adaptation of the 8-Item Perceived Organizational Support Scale (19). Respondents were asked to assess the degree to which they agreed the organization cared about their satisfaction, well-being, and extra efforts and contributions, leading to a total possible score of 3 to 15.
Work control (autonomy) was measured using a single-item measure from the Veterans Affairs Annual Work Experience Survey 2018 version asking the degree to which employees agreed they had control over how their work is carried out and had input into decisions that affected their work (5-point Likert Scale) (18).
Due to financial shortfalls from cancelling of elective procedures, compensation reductions were implemented for most of the medical center employees in May 2020 and were graduated based on income. Respondents were asked the degree to which they agreed that given the financial challenges the organization was facing, the compensation reductions were fair, transparent, and equitable (5-point Likert Scale).
Respondents also chose their major general work-related stressors such as increased responsibilities or job demands, reduced productivity, exposure to COVID-19, and reduced income. Clinicians selected their major clinical stressors such as inadequate PPE, adapting to telemedicine, scope of practice concerns, and testing shortages.
Non-work-related factors
Individual resilience was measured using the 2-item CD-RISC-2 scale (20), which results in scores ranging from 0-8 with 8 indicating the highest resilience. Respondents selected their top non-work stressors such as childcare, loneliness or social isolation, and societal response to COVID-19. Gender and family status were also collected.
Statistical analysis
WBI score, resilience score and counts of overall, clinical, work, and non-work stressors were calculated and stratified by ACT membership status. Frequency and percentages of major work and non-work-related stressors by ACT membership were calculated. Chi-Square and t-tests were conducted to determine whether ACT groups differed along the main variables of interest. Multivariate regression analysis using listwise deletion was conducted to examine whether ACT membership was associated with lower distress while controlling for the work environment characteristics described under the independent variables section. We calculated standardized regression coefficient to compare adjusted R-square values for goodness of fit.
Results
A total of 1,130 respondents took the survey with a response rate of 18 percent (participants who participated/total of contacted participants). Participants who did not report their ACT membership status excluded from the analysis (n=335), leaving a final sample size of 1,070 respondents (55 ACT members, 1,015 non-ACT members).
ACT team members had significantly better performance on several dimensions compared to non-ACT members, Table 2. On average, ACT members on average felt greater support from their organization, specifically that they (M =9.22, SD =4.18), believed their organization recognized their effort (M =3.35, SD =0.98, P<0.05) and showed concern for them (M =3.43, SD =1.27, P<0.05). ACT members also had higher resilience scores (M =7.02, SD =1.14, P<0.05) and felt a greater sense of community at work (M =4.15, SD =1.07, P<0.05). Moreover, 20% fewer ACT members reported loneliness or social isolations (χ2=4.20, P<0.05) as a major stressor. ACT members were more likely to report heavy workloads and long hours (χ2=11.87, P<0.01), increase job demands or responsibilities (χ2=4.06, P<0.05) and childcare (χ2=6.22, P<0.05) as major stressors. ACT members also reported more stress associated with the perception that patients were receiving poor care or treatment (χ2=8.62, P<0.01). Lastly, ACT members had a greater percentage of female members compared to non-ACT members (χ2=11.32, P<0.05).
Table 2
| ACTa | Non-ACTb | Test-statistice | ACT performancef | |
|---|---|---|---|---|
| N | 55 | 1,015 | ||
| Wellbeing index score, mean (SD)c | 4.29 (2.12) | 4.17 (2.32) | −0.37 | − |
| Perceived organizational support score, mean (SD) [3–15]c | 9.22 (4.18) | 8.38 (4.04) | −1.51 | + |
| Org Support-Recognizes extra efforts [1–5], mean (SD)c | 3.35 (0.98) | 2.93 (1.21) | −2.11* | + |
| Org Support-Shows little concern for me (reverse scored) [1–5] mean (SD)c | 3.43 (1.27) | 3.14 (1.19) | −1.67* | + |
| Sense of Community at Workc | 4.15 (1.07) | 3.89 (1.04) | −1.69* | + |
| Moral distress score, mean (SD)c | 1.45 (1.61) | 1.42 (1.55) | −0.15 | − |
| Work control score, mean (SD)c | 3.52 (1.22) | 3.45 (1.15) | −0.41 | + |
| Decision Involvement score, mean (SD)c | 3.37 (1.29) | 3.31 (1.24) | −0.30 | + |
| Resiliency score, mean (SD)c | 7.02 (1.14) | 6.61 (1.25) | −2.29* | + |
| Perceived equity of pay cut, mean (SD)d | 1.92 (1.44) | 1.82 (1.26) | −0.55 | + |
| % Heavy Workload or Long Hoursd | 52.73 | 30.05 | 11.87** | − |
| % Increased Job Demands/Responsibilitiesd | 58.18 | 43.55 | 4.06* | − |
| % Patients receiving poor treatmentd | 25.45 | 11.63 | 8.62** | − |
| % High Risk of COVID Exposured | 23.64 | 25.91 | 0.26 | + |
| % Loneliness/social isolation as a major stressord | 20.00 | 32.32 | 4.20* | + |
| % Childcare as a major stressord | 34.55 | 20.20 | 6.22* | − |
| Genderd | 11.32* | |||
| % Female | 67.27 | 62.17 | ||
| % Male | 14.55 | 17.34 | ||
| % Prefer not to answer | 7.27 | 12.41 | ||
| % Self-describe | 3.64 | 0.39 |
*P<0.05, **P<0.001. a, ACT member; b, non-ACT member; c, one tail t-test; d, chi-2 test; e, Bivariate test determining the association between ACT membership and the predicting variables included in the Multivariate Regression model; f, + indicates better performance by the ACT, − indicates worse performance by the ACT. ACT, Accountable Care Team; SD, standard deviation.
In the multivariate regression analysis, ACT membership was not significantly associated with overall distress scores, Table 3, failing to support Hypothesis 1. When controlling for ACT membership in the multivariate regression model, Advanced Practice Providers (β=0.467 P<0.01), and Clinical Support Staff (β=0.639, P<0.001) reported higher distress scores. Male employees reported better Well-Being Index Scores compared to females (β=-0.350, P<0.05). Moreover, higher Moral Distress Frequency (β=0.293, P<0.001), heavy workload or long hours (β=1.407, P<0.001), increased job demands or responsibilities (β=0.759, P<0.001), high risk of COVID Exposure (β=0.334, P<0.05), and loneliness or social isolation (β=0.649, P<0.001) were associated with increased distress. On the other hand, those who had a higher sense of work control (β=−0.235, P<0.001), believed the pay cut was fair or equitable (β=−0.140, P<0.01), and reported higher resiliency (β=−0.216, P<0.001) reported lower distress scores. Standardized regression coefficient indicated that heavy workload or long hours had the largest negative impact, while work control served as the best mitigating factor.
Table 3
| Variable | Coef. (95% CI) | b |
|---|---|---|
| Accountable Care Team membership (0–1) | −0.136 (−0.658 to 0.385) | −0.013 |
| Job category | ||
| Administration & Non-Clinical, Referent | [Reference] | |
| Advanced Practice Provider | 0.467 (0.124 to 0.810)** | 0.086 |
| Clinical Support Staff | 0.639 (0.287 to 0.990)*** | 0.105 |
| Nurse | 0.280 (−0.110 to 0.670) | 0.042 |
| Other | 1.048 (−0.395 to 2.490) | 0.034 |
| Physician | −0.145 (−0.498 to 0.208) | −0.025 |
| Trainee Resident/Fellow | 2.067 (−0.210 to 4.344) | 0.043 |
| Perceived organizational support score [3–15] | −0.014 (−0.207 to 0.178) | −0.021 |
| Org. Support-Recognizes extra efforts [1–5] | −0.018 (−0.349 to 0.313) | −0.009 |
| Org. Support-Shows little concern for me (reverse scored) [1–5] | −0.082 (−0.381 to 0.217) | −0.043 |
| Sense of Community Work | −0.014 (−0.136 to 0.107) | −0.007 |
| Moral Distress Frequency [1–5] | 0.293 (0.215 to 0.371)*** | 0.200 |
| Work Control [1–5] | −0.235 (−0.363 to −0.107)*** | −0.119 |
| Decision involvement [1–5] | 0.008 (-0.112 to 0.128) | 0.004 |
| Heavy Workload or Long Hours (0–1) | 1.407 (1.149 to 1.665) *** | 0.295 |
| Resilience (0–8) | −0.216 (−0.305 to −0.127)*** | −0.117 |
| Perceived Fairness/Equity of Pay cut (0–4) | −0.140 (−0.245 to −0.034)** | −0.078 |
| Increased Job Demands/Responsibilities (0–1) | 0.759 (0.506 to 1.013)*** | 0.167 |
| Patients receiving poor treatment (0–1) | −0.111 (−0.450 to 0.229) | −0.017 |
| High Risk of COVID Exposure (0–1) | 0.334 (0.065 to 0.603)* | 0.067 |
| Loneliness/social isolation as a major stressor (0–1) | 0.649 (0.421 to 0.876)*** | 0.137 |
| Childcare as a major stressor (0–1) | 0.039 (−0.216 to 0.294) | 0.007 |
| Gender | ||
| Female | [Reference] | |
| Male | −0.350 (−0.650 to −0.050)* | −0.060 |
| Prefer not to answer | −0.338 (−0.696 to 0.020) | −0.045 |
| Self-describe | 0.192 (−1.136 to 1.522) | 0.007 |
| Adjusted R 2 | 0.4963 |
*P<0.05, **P<0.01, ***P<0.001. WBI, Well-Being Index; Coef., coefficient; CI, confidence interval; b, standardized regression coefficient.
Discussion
The strength of this study is to evaluate the effectiveness of an intervention during a state of crisis, as a possible mechanism for protecting against diminished well being. In this study we found mixed support for the ACT model to serve as “psychological PPE” for healthcare workers during the COVID-19 pandemic. Despite the non-ICU COVID-19 units also being ACT units, the ACT members felt more supported by the organization, had a better sense of community at work and were less likely to report loneliness and social isolation as a major stressor. Taken together, these results suggest that ACT members felt more connected and had greater sense of belongingness at work compared to non-ACT members. It is not entirely surprising that ACT members also reported heavy workloads and additional responsibilities compared to non-ACT members who may have been on non-COVID designated units. Our results support suggest that participation in the ACT model is associated with a reduction in specific types of stressors and better work environment characteristics among healthcare workers during COVID-19 even in the nascent phases of the intervention. Loneliness was found to be a major driver of distress, so fostering a sense of connection at work represents an important opportunity to move the needle on well-being. ACT members also had greater resilience compared to others, though the cross-sectional nature of this study does not allow us to understand causality or directionality of the relationship.
ACT membership was not associated with improved overall distress scores, however. This is unsurprising given that some of the ACT units were also serving as COVID-19 units. Increased job demands and responsibilities and heavy workload were the top two drivers of overall distress for the entire health system population (17), and it is likely that COVID-19 units had increased demands of patient care relative to non-COVID units. Because ACT members reported higher incidence of heavy workload and increased responsibilities, it is likely that these factors counteracted the many benefits of ACT membership leading to lack of significance in the relationships between ACT membership and overall distress. Additionally, employees on these units may have been more likely to experience stress related to poor treatment of patients due to COVID-related restrictions, such as the inability to have one’s family present during their illness or death. There is also the possibility that participating in the ACT intervention itself contributed to additional responsibilities such as extra meetings and additional process improvement projects. While we attempted to control for a number of COVID-related stressors, it is possible that we failed to control for all factors that are unique to those units.
In addition to COVID-19 related stressors, ACT membership may have failed to mitigate overall distress due to early stage of the intervention when the pandemic commenced. At the time of survey, none of the ACT units had completed both the leadership and problem-solving training and all were still in the development phase. Although the initial CPT training lasts about six months, an ACT is not considered fully mature until it had also completed the LDO training and had hardwired the culture of systems-based problem solving. While two teams had the opportunity to practice problem solving before COVID-19, most teams in this study were still in the early stage of cultural adaptation. We would expect that teams with more time to use systems-based problem solving outside of the pandemic would yield significantly better distress scores.
Additionally, the gender composition of the ACT teams may have attenuated the benefits of ACT membership on overall distress scores. ACTs had 8% more female members compared to non-ACT groups. Because females were statistically significantly more distressed when controlling for other factors, this gender composition may also explain why more ACT members reported childcare as a major stressor.
Since ACT teams is a relatively new concept, in addition to our research, currently there are only two other studies examining the benefits of this work structure. Both studies incorporate an ACT intervention to determine how this healthcare format contributes to teamwork efficiency (2,5). Different from previous scholarship, our work focuses on wellbeing and the performance of ACTs under crisis conditions. We examine the role of ACT teams in healthcare workers’ distress within the midst of a global pandemic. To our knowledge, our study uses the largest sample and incorporates all types of hospital employees previously unstudied in the aforementioned studies, such as clinical support staff and non-clinical staff).
There are several limitations to this study. First, the survey used for this analysis was administered at the beginning of our organization’s ACT implementation journey. This training is designed to empower ACT members to function as a high-performing, interprofessional team with the tools needed to solve problems within their microsystem. Thus, we expect the benefits to be fully realized once the training is completed and the ACT is mature. Additionally, given the cross-sectional nature is study, we cannot infer causality of the ACT intervention and findings may not be generalizable to other organizations or contexts. It is possible that the members of an ACT unit have different intrinsic qualities that might influence the other variables of interest. Longitudinal data collection is currently underway. While our early results suggest the ACT intervention is associated with better performance on elements of employee well being such as a sense of community and support at work, it is important to consider other work-related factors that may counteract these positive benefits. Such an intervention alone may not be able to counteract the negative effects of low staffing levels, poor work design or role overload. Additionally, as participation in the intervention requires additional time and effort, the organization must ensure that employees have enough support and time to engage rather than adding to their existing workload. Without proper support for the intervention, the increased workload of meeting and problem-solving within the ACT, and the additional responsibilities of training may counteract the many positive benefits of the intervention. Organizations need to consider protected time and appropriate staffing levels to support participation in an ACT. Furthermore, as ACT members were more likely to report childcare as a major stressor, organizations need to consider what supports are in place for working parents, such as on-site childcare services or flexible working arrangements.
In conclusion, early results suggest ACT membership may be beneficial to some domains of employee well-being. Future study is needed to evaluate the impact of fully mature ACTs as well as the impact of additional workloads on team member distress.
Acknowledgments
Funding: This study was funded by a grant from the ProAssurance Corporation, awarded to David A. Rogers.
Footnote
Provenance and Peer review: This article was commissioned by the editorial office, Journal of Hospital Management and Health Policy for the series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at: https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-70/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-70/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-70/coif). The series “Shaping Tomorrow’s Healthcare Systems: Key Stakeholders’ Expectations and Experiences” was commissioned by the editorial office without any funding or sponsorship. KAM served as an unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring the questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the University of Alabama at Birmingham (No: IRB-300005398) and informed consent was taken from all of the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Framework for action on interprofessional education and collaborative practice [Internet]. Health professions networks nursing & mdiwifery human resources for health. 2010 [cited 2021 Sep 14]. Available online: http://apps.who.int/iris/bitstream/handle/10665/70185/WHO_HRH_HPN_10.3_eng.pdf;jsessionid=1B651EAE33A5D3214A22B6E4418D1E6A?sequence=1
- Marrone SR. Perioperative accountable care teams: Improving surgical team efficiency and work satisfaction through interprofessional collaboration. J Perioper Pract 2018;28:223-30. [Crossref] [PubMed]
- Kastor JA. Accountable Care Organizations at Academic Medical Centers. N Engl J Med 2011;364:e11. [Crossref] [PubMed]
- Joseph ML. Organizational Culture and Climate for Promoting Innovativeness. J Nurs Adm 2015;45:172-8. [Crossref] [PubMed]
- Kara A, Johnson CS, Nicley A, et al. Redesigning inpatient care: Testing the effectiveness of an accountable care team model. J Hosp Med 2015;10:773-9. [Crossref] [PubMed]
- O’Leary KJ, Johnson JK, Manojlovich M, et al. Redesigning systems to improve teamwork and quality for hospitalized patients (RESET): study protocol evaluating the effect of mentored implementation to redesign clinical microsystems. BMC Health Serv Res 2019;19:293. [Crossref] [PubMed]
- Reith TP. Burnout in United States Healthcare Professionals: A Narrative Review. Cureus [Internet]. 2018 Dec 4; Available online: https://www.cureus.com/articles/16398-burnout-in-united-states-healthcare-professionals-a-narrative-review
- American Hospital Association. Trendwatch hospital and health systems workforce strategic planning [Internet]. 2020 [cited 2020 Oct 1]. Available online: https://www.aha.org/system/files/media/file/2020/01/aha-trendwatch-hospital-and-health-system-workforce-strategic-planning2_0.pdf
- MedScape. US and International Physicians’ COVID-19 Experience Repor. 2020.
- Institute for Healthcare Improvement. “Psychological PPE”: Promote Health Care Workforce Mental Health and Well-Being. 2020.
- Dyrbye LN, Satele D, Sloan J, et al. Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med 2013;28:421-7. [Crossref] [PubMed]
- Dyrbye LN, Satele D, Shanafelt T. Ability of a 9-Item Well-Being Index to Identify Distress and Stratify Quality of Life in US Workers. J Occup Environ Med 2016;58:810-7. [Crossref] [PubMed]
- Tawfik DS, Profit J, Morgenthaler TI, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc 2018;93:1571-80. [Crossref] [PubMed]
- Dyrbye LN, Johnson PO, Johnson LM, et al. Efficacy of the Well-Being Index to identify distress and stratify well-being in nurse practitioners and physician assistants. J Am Assoc Nurse Pract 2019;31:403-12. [Crossref] [PubMed]
- Hall LH, Johnson J, Watt I, et al. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. Harris F, editor. PLoS One 2016;11:e0159015.
- Beresin EV, Milligan TA, Balon R, et al. Physician Wellbeing: A Critical Deficiency in Resilience Education and Training. Acad Psychiatry 2016;40:9-12. [Crossref] [PubMed]
- Meese KA, Colón-López A, Singh JA, et al. Healthcare is a Team Sport: Stress, Resilience, and Correlates of Well-Being Among Health System Employees in a Crisis. J Healthc Manag 2021;66:304-22. [Crossref] [PubMed]
- U.S. Department of Venterans Affairs. National center for organizational development. VA All Employee Survey. 2018.
- Eisenberger R, Huntington R, Hutchison S, et al. Perceived organizational support. J Appl Psychol 1986;71:500-7. [Crossref]
- Vaishnavi S, Connor K, Davidson JRT. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacological trials. Psychiatry Res 2007;152:293-7. [Crossref] [PubMed]
Cite this article as: Meese KA, Dobbins CF, Colón-López A, Van Pelt F, Rogers DA, Flood KL. Accountable care team membership and distress: is accountable care team membership associated with lower distress during a crisis? J Hosp Manag Health Policy 2022;6:22.

