Use of a Key Drivers Diagram in preparation for COVID-19 at an urban, academic anesthesiology department
Introduction
The first patient in the US known to be infected with COVID-19 was identified on January 20th, 2020 in the State of Washington (1), followed by a February, 2020 outbreak in the Seattle, Washington area. Early studies suggested that cities with a high degree of international traffic were at particular risk (2,3). Washington, DC boasts three international airports within a 30-mile radius and has a population density of over 10,000 people per square mile. In early March, outbreaks in neighboring New York, NY and Boston, MA reinforced the urgency to conserve hospital resources for an impending outbreak in Washington, DC. The first confirmed COVID-19 case in Washington, DC was on March 7, 2020.
Early experience with COVID-19 implicated community transmission as responsible for the majority of infections. This stands in contrast to the experience from previous coronavirus outbreaks, such as SARS-CoV and MERS-CoV, where the majority of transmission was nosocomial, and associated with aerosol-generating procedures in affected patients. In those outbreaks, healthcare workers that were involved in manipulating the airway, including anesthesiologists, intensivists and emergency medicine physicians were at significantly higher risk of morbidity and mortality (4). Accordingly, given the likely increased infectivity of COVID-19, and the inability to reliably identify asymptomatic individuals capable of virus transmission, aggressive intervention was necessary to prevent similar or worse spread of COVID-19 among healthcare workers responsible for airway management.
The reporting of COVID-19’s devastating impact on other first-world healthcare systems, alongside a rapid influx of new research of unclear significance created a sense of uncertainty and anxiety about how to precisely intervene adequately on a local level. Our anesthesiology department drew on previous successful experiences with healthcare quality improvement (QI) in clinical process improvement as well as institutional coordination efforts to promote a unified methodology to guide preparations for an effective, consistent, and aligned COVID-19 response.
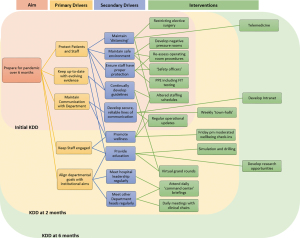
A Key Drivers Diagram (KDD) is a visual display of what contributes to the achievement of a project aim (5). It is a useful tool for communication that, combined with other measures, can provide stakeholders with a clear view of simultaneous processes. It also allows for better identification of strategic interventions that can be measured to quantify progress. It has been used to coordinate national safety initiative programs (6), and even to plan public health strategy on a government level (7).
We present the following article in accordance with the SQUIRE and MDAR reporting checklists (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-5/rc) (8).
Methods
The George Washington University hospital is a 431-bed urban, quaternary care hospital. Prior to the COVID-19 pandemic, our anesthesiology department provided support for approximately 25,000 surgeries a year, and employed a clinical staff of 78 faculty, trainees and allied health professionals.
On February 27, 2020, a week before the first COVID-19 case was diagnosed in Washington, DC, Department leaders (Chair, Director of Clinical Operations, Director of Quality, Director of Cardiac Anesthesiology) met to discuss the possible impact of the impending pandemic on our department. A KDD (Figure 1) was developed to define strategic goals for our preparation. They identified five primary drivers that would guide preparations over an anticipated two-months response: (I) protect patients and staff; (II) keep up-to-date with changes; (III) keep staff engaged; (IV) maintain communication; and (V) align departmental goals with broader aims. These drivers were discussed at weekly departmental meetings, and progress was shared with the Anesthesiology Department. Strategies and metrics were also added to or removed from the KDD at this meeting, and interventions developed by appointed sub-committees.
This study received a determination of “not human research” from the George Washington University Institutional Review Board.
Primary driver 1: protect patients and staff
Our interventions focused on adequate distancing of both staff and patients, enhancing environmental safety, and providing appropriate personal protective equipment (PPE). Initial steps included masking staff (early March 2020) and patients (late March), developing exposure protocols for staff (late March), limiting ingress and egress to the facility with temperature checks and exposure risk assessments (early April), limiting visitors (mid-April) with delineated exceptions (e.g., partner of a laboring obstetric patient) testing prior to surgery and hospital admission (mid-April), and telemedicine options (July). As the scale of pandemic worsened, our institution was the first in the region to cancel elective procedures and surgeries, starting the week of March 16, 2020. During the first week of reduced surgical services, 282 cases were cancelled (67%).
In response to this reduction in caseload, a sub-committee of senior attendings was tasked with designing a new work schedule. The perioperative anesthesiology workforce was divided into three teams with an equal skills-mix of attendings, residents and certified anesthesia assistants. Each team worked a one-week rotation (Monday through Sunday), followed by a week of clinical back-up with a low burden of in-hospital duty, and lastly a week with no clinical assignment. Effectively, each provider was exposed clinically for one week, followed by a two-week period of limited to no clinical exposure, which functioned as a built-in isolation period. This was in keeping with the 14-days period suggested by the Center for Communicable Diseases (CDC) to monitor for development of signs and symptoms after potential exposure to COVID-19(9).
A minimum of two anesthesiology attendings were scheduled to be in the hospital at all times with backup coverage as needed. A few staff were excused entirely from clinical duties due to personal health issues that put them, or a member of their household, at increased risk for morbidity or mortality from COVID-19.
Modifications were made to existing operating room (OR) procedures, with one large OR designated for COVID-19 emergency surgical cases. Non-essential equipment was removed, and the remainder covered with clear plastic draping to minimize contamination. Further modifications were made to the anesthetic machine breathing circuit to protect both the machine and the patient from potential contamination. These changes were replicated in our Labor and Delivery Unit OR, in consultation with the Obstetric team. We liaised Hospital engineers to create negative-pressure, filtered anterooms for a COVID-19 designated OR and select procedural locations. Engineers also provided measurements for air changes per hour to enforce safe periods after the conduct of aerosolizing procedures or for commencing terminal room cleaning.
Regarding equipment, beginning February 28, 2020, all staff were qualitatively fit tested to ensure proper N95 mask designation (10). Additional fit testing personnel were brought on site to support training. A senior member of the Department was tasked with keeping dynamic inventory of PPE stock, and sourcing more sophisticated equipment, such as powered air purifier respirators (PAPRs). Emergency plans for sterilization and re-use of N95 masks, as well as re-purposing of OR ventilators for intensive care use were also considered.
Recognizing that the application of multiple new guidelines and procedures, such as donning and doffing of PPE, might be daunting for our providers, we worked with the Professional Development and Education team in the Hospital to develop “safety officers”. These new members of emergency response teams were tasked with education around appropriate PPE and PAPR use, and were present at all airway interventions to guide and encourage safety protocol compliance.
Primary driver 2: keep up-to-date with changes
Members of the Department, including trainees, were encouraged to explore evolving evidence about COVID-19, as well as consult with their colleagues from other affected areas for practical advice. They were then assigned identified topics upon which to draft guidelines, incorporating information from national organizations, such as the American Society of Anesthesiologists (ASA), Anesthesia Patient Safety Foundation (APSF) and the Centers for Disease Control (CDC), in addition to expert opinion and pre-print journal articles. Guidelines were substantially revised and new topics added on a weekly basis for the first several weeks as a result of evolving research, hospital simulations, and the introduction of first-hand experiences.
Monday morning walk rounds in the OR were initiated to acquaint the weekly, incoming clinical team with the latest clinical developments, to apprise them of new guidelines, and to ensure their comfort with new clinical equipment or PPE. Daily checklists were created to ensure emergency response equipment was available.
Primary driver 3: maintain communication
The Department Chair and Director of Clinical Operations offered daily, on-site, administrative oversight to ensure continuity of leadership. With the change in work schedules, and three separate shifts, it was important to ensure continuity via regular operational updates. A brief Monday morning teleconference, prior to the clinical walk rounds, kept all teams updated on hospital status and other relevant issues. Daily, and then weekly, consolidated e-mail kept the Department informed of events during the most intense months of the crisis. As the situation normalized, email communication was reserved for significant changes, or compliance reminders, to existing protocols. Department text messages, initially heavily utilized, were later intentionally kept to a minimum to avoid being intrusive.
Prior to the pandemic, the departmental intranet had fallen out of use. Working with hospital IT, we re-designed the site to securely host new guidelines, policies and other resources. Resources included important hospital phone numbers, schedules, and copies of department-wide communication.
Primary driver 4: keep staff engaged
Synchronous education opportunities in the form of simulation and weekly grand rounds were developed, and a list of on-line resources promoted asynchronous learning.
Simulation was in-situ, both scheduled and impromptu, and targeted to physicians, nurses, respiratory therapists and other members of the emergency response, including safety officers. It was facilitated by instructors from the University Simulation Center. Mannequins, ventilators, monitors, PPE and other supplies were used for low-fidelity simulated airway emergencies. Hospital code simulations occurred daily over the last two weeks of March in unoccupied hospital ward rooms. From mid-March to mid-April, weekly OR emergency drills were conducted, and the Labor and Delivery suite simulated emergency cesarean deliveries twice daily. Debriefs occurred after every session, and attendance was noted. From mid-March, weekly Grand Rounds were broadcast to members of the department who were at home via the intranet. Example topics covered over the weeks included intensive care ventilation and management, donning and doffing of PPE, a morbidity and mortality review of COVID-19 patient management, and ethical dilemmas.
A selection of curated educational supplements, including primary sources, article summaries and podcasts were housed on the department intranet (Table 1). Recorded simulation sessions, such as a COVID-19 positive floor intubation, were available for staff review. Opportunities for clinical research were also developed, particularly retrospective studies that could be performed remotely.
Table 1
| Variable | Details |
|---|---|
| Communication | |
| Contact numbers | Archive of COVID-19 related emails |
| Link to Department ShareDrive | Adjusted clinical schedules |
| Psychiatry resources for COVID-related stress | |
| Guidelines | |
| Airway management | Neonate LDR delivery and NICU |
| Code blue checklist | Nitric oxide policy ICU |
| Code blue | Obstetric emergency cesarean delivery |
| Critical care | Obstetric emergency flowchart |
| PPE: Donning & Doffing | Obstetric patient plan |
| EMed airway | Personal decontamination plans |
| ENT management | POCUS |
| Ethics code recommendation | Proning |
| Ethics document | Surgery in OR |
| Exposure | Testing for surgery and procedures |
| Extended use and reuse | Tracheostomy checklist |
| Intubation note | Transport |
| Key communications | Trauma |
| Websites | |
| American College of Physicians: COVID-19 | Hospital: ICU Primer |
| American College of Physicians: Hospital Medicine Updates | Hospital: COVID Situation Report |
| Anesthesiology: Coronavirus | Hospital: Research Guides |
| EMCrit resources for COVID-19 | Mt Sinai Hospital: COVID ICU Guide |
| DC Department of Health: COVID tracker | Society of Critical Care Medicine: Basic ICU Management |
PPE, personal protective equipment; EMed, emergency medicine; ENT, ear/nose/throat; LDR, labor and delivery room; NICU, neonatal intensive care unit; POCUS, point-of-care ultrasound; EMCrit, emergency medicine and critical care.
From a wellness perspective, from mid-March through April, weekly Friday afternoon wellbeing check-ins were facilitated by a psychiatrist in conjunction with Department leaders. These sessions afforded a virtual space to fraternize, commiserate and encourage.
Primary driver 5: align departmental goals with institutional aims
New departmental leadership responsibilities included four-times daily hospital command center briefings with hospital administrative leadership, daily meetings with clinical chairs, three-times weekly expanded hospital leadership updates, and weekly “town-hall” question-and-answer sessions with front-line workers. This allowed for continuity of the Department’s clinical response and ensured alignment of activities with broader institutional strategic initiatives in response to COVID-19. Interdisciplinary collaborations in guideline creation led to a cohesive institutional approach for a broad array of clinical COVID-19 considerations.
Departmental goals included consideration for the financial impact of COVID-19 loss of surgical revenue, and system-wide reductions in productivity. Mitigation strategies to address financial losses were considered only after addressing the physical and emotional safety of patients and staff. Early interventions included elimination of work-related travel and continuing medical education funds until 2021. Providers were also required to keep assigned vacation slots.
Methods of evaluation
Specific metrics were associated with each key driver, over the initial two-month time period, to enable us to evaluate efficacy. For driver 1, safety measures include the number of staff who contracted COVID-19. For driver 2, as a measure of keeping up-to-date with information, the number of new guidelines developed were recorded. For driver 3 and 4, staff engagement and robust communications were measured by attendance at weekly virtual grand rounds. Finally, for driver 5, external engagement was tracked by the number of meetings between departmental leadership with other leaders.
Statistical analysis
We use run charts to objectively evaluate the process improvements in our department over time. They are useful for early detections of signals of improvement or degradation, and can differentiate non-random from random shifts and trends(11). A significant shift is identified by ≥6 consecutive points above or below the median, and a trend by ≥5 consecutive points going all up or down.
Results
As of November 2020, no members of our department have been diagnosed with COVID-19, or required leave as a consequence of possible exposure. All data collected was included in analysis.
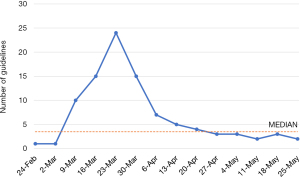
Figure 2 displays the number of new or revised guidelines produced by our department per week. There was a steep increase activity in this area over the start of March, reaching a peak of 24 either newly written or revised guidelines in the last week of March. A median of 3.5 guidelines were written or revised per week, and the run chart shows a statistically significant positive shift and trend of activity over this period.
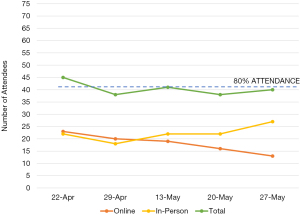
Figure 3 shows attendance of physicians (attendings and residents) at the grand round events over this period. Grand rounds were initially cancelled at the start of the pandemic, and only recommenced at the end of April. Further, there was no grand round at the start of May due to a monthly scheduled faculty meeting. Attendance was generally around the 80% mark (40.5; two-thirds of 76 staff), with both online and in-person approaches utilized.
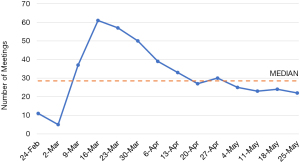
Finally, Figure 4 is the number of official meetings attended or conducted by departmental leadership. There were a median of 28.5 meetings over this period, and a positive shift and trend were also identified.
Discussion
Our department was able to adapt to meet a complex array of technical and non-technical challenges by early adoption of a KDD to perform and evaluate parallel process improvement with a systems-based approach (12). In the early phases of development, this model helped to emphasize the interrelation between seemingly disparate elements of our response, and identify potential inefficiencies and need for collaboration with other departments. The identification of strategic priorities allowed for efficient delegation of staff and expertise, and ensured role clarity and good teamwork. The use of run charts provided an accessible and clear indicator of dynamic progress, and enabled our department to set achievable aims to match strategic goals. Further, the results displayed only represent a fraction of the multiple rapid plan-do-check-act cycles that were instituted through this period.
Taking intentional steps to protect our staff and patients was identified early as a priority, and none of our staff having contracted COVID-19 was a good reflection of that success. Measures such as cancelling elective surgical procedures, education around appropriate PPE use, ensuring stocks of equipment and distancing via altered work scheduling were key to achieving this. Our decision to cancel elective surgery was one day prior to the Washington, DC’s advice to halt elective surgery (13), several days in advance of a similar decision from another local hospital system (14) and weeks in advance of many privately-operated surgical centers in the area. Being the first to commit to elective case cancellations risked the loss of market share from referring physicians and patients. The need to fit test all staff for respirator (i.e., N95 masks) use at the outset of the pandemic, despite routine annual requirements for fit testing, was required due to the influx of new respirator makes driven by increased global demand and limited access to our institution’s preferred make.
These measures helped reassure staff and develop confidence in leadership’s commitment to a culture of safety. Different activities also identified similar problems, which therefore had unified solutions. For instance, simulation and then subsequent clinical experience with the first COVID-19 case in the OR led to a dynamic evolution of both technical and non-technical modifications: for example, single-use equipment and supplies were made more readily available in order to reduce interaction between ‘clean’ and ‘dirty’ environments, and communication had to be enhanced with the use of easily disinfected portable two-way radio transceivers that could be audible over the noise generated by PAPRs.
Keeping up-to-date with evidence allowed the department to anticipate contingencies, set priorities dynamically and re-evaluate these periodically. It also gave trainees practical insight into how guidelines are created. The statistically significant increased activity in this area reflected the department enthusiasm at being asked to participate in executive functions, which also allowed departmental leadership to assume an oversight role, maintaining situational awareness.
Continual professional education was an intentional focus for our department as we felt it at high risk of being overlooked during an evolving crisis. Attendance remained fairly constant throughout the period observed, and staff took advantage of the virtual option in order to participate. The grand round also gave us the opportunity to speak to other departments, learn from collective experience, and identify blind spots in our approach.
Identifying the granular components required to make our response effective also helped guide our leadership response to the pandemic, which is reflected in the number of official meetings that occurred over this period. These included inter-departmental strategic planning, research, and operational updates. This reflected a heightened engagement by departmental leadership to provide clarity and direction during a time of uncertainty, and helped to develop trust with institutional leadership. Aside from local meetings, we were also represented at regional and national conferences about the pandemic, such as the DC Mayoral town-hall, Specialty Society Meetings and other leadership conferences. These external meetings helped to contextualize what was happening in our institution against a larger backdrop.
Evaluation of the KDD was limited by several notable factors. The KDD evolved over time, and the time-sensitive nature of interventions limited mitigation of design flaws. For example, there was no control group in our study. All members of the team participated in the intervention; therefore, it is not certain that the KDD influenced reported metrics, such as quantity of guidelines or meetings attended. Furthermore, the authors both designed and participated in the intervention; hence, the authors were not blinded. However, this impact was reduced by assigning collection and interpretation of the data to a non-clinical research assistant (GH).
Conclusions
Embedding QI methodology into daily clinical practice is a dynamic process, and we found that the use of a KDD model helped to evaluate and communicate our progress through the pandemic. It enabled us to view disparate elements of our response as interrelated components, promoting an effective and consistent response. While often used in large organizations, we feel that it presents a helpful model for developing even a departmental response to a pandemic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SQUIRE and MDAR reporting checklists. Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-5/rc
Data Sharing Statement: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-5/dss
Peer Review File: Available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-5/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jhmhp.amegroups.com/article/view/10.21037/jhmhp-21-5/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study received a determination of “not human research” from the George Washington University Institutional Review Board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382:929-36. [Crossref] [PubMed]
- Schuchat A. Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morb Mortal Wkly Rep 2020;69:551-6. [Crossref] [PubMed]
- Rocklöv J, Sjödin H. High population densities catalyze the spread of COVID-19. J Travel Med 2020;27:taaa038.
- Zucco L, Levy N, Ketchandji D, et al. Perioperative Considerations for the 2019 Novel Coronavirus (COVID-19). Epub Feb 12, 2020.
- Driver Diagram | IHI - Institute for Healthcare Improvement. Accessed February 4, 2021. Available online: http://www.ihi.org:80/resources/Pages/Tools/Driver-Diagram.aspx
- IHI Improving Perinatal Care Driver Diagram | IHI - Institute for Healthcare Improvement. Accessed February 4, 2021. Available online: http://www.ihi.org:80/resources/Pages/Changes/IHIImprovingPerinatalCareDriverDiagram.aspx
- Using Driver Diagrams to Map a National COVID-19 Response. Accessed February 4, 2021. Available online: http://www.ihi.org/communities/blogs/africa-using-driver-diagrams-to-map-a-national-covid-19-response
- Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016;25:986-92. [Crossref] [PubMed]
- Patel A, Jernigan DB. Initial Public Health Response and Interim Clinical Guidance for the 2019 Novel Coronavirus Outbreak – United States, December 31, 2019-February 4, 2020. MMWR Morb Mortal Wkly Rep 2020;69:140-6. [Crossref] [PubMed]
- Fraser V. Respirators and Fit Testing. Infect Control Hosp Epidemiol 1996;17:633-5. [Crossref] [PubMed]
- Perla RJ, Provost LP, Murray SK. The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf 2011;20:46-51. [Crossref] [PubMed]
- Goldman D. How do you use a Driver Diagram? Institute for Healthcare Improvement. Accessed April 14, 2021. Available online: http://www.ihi.org/education/IHIOpenSchool/resources/Pages/Activities/GoldmannDriver.aspx
- Recommendations on limitations of Elective and Non-urgent Medical and Dental Procedures. DC Health Regulation and Licensing Administration. March 17, 2020. Accessed April 14, 2021. Available online: https://dchealth.dc.gov/sites/default/files/dc/sites/doh/page_content/attachments/Letter%20-%20Elective%20Procedures.FINAL_.pdf
- MedStar Health Postponing Elective Procedures and Surgeries starting Thursday 19 March in response to COVID-19. MedStar Health. March 17, 2020. Accessed April 14, 2021. Available online: https://www.medstarhealth.org/mhs/2020/03/17/medstar-health-postponing-elective-procedures-and-surgeries-starting-thursday-march-19-in-response-to-covid-19/
Cite this article as: Parr KG, Ho G, Burnette M, Gould J, Petinaux B, Sherman M, Berger J. Use of a Key Drivers Diagram in preparation for COVID-19 at an urban, academic anesthesiology department. J Hosp Manag Health Policy 2022;6:3.