
Team strategies to manage vulnerable patients’ complex health and social needs: considerations for implementing team-based primary care
Introduction
Primary care reform efforts have promoted team-based care as an approach to improve access to high-quality primary care services for more patients and improve patients’ health outcomes (1-4). Team-based primary care has broadly been conceptualized as providing comprehensive services for individuals, families and communities by health professionals, caregivers, and community services “who work collaboratively on shared goals within and across settings to achieve care that is safe, effective, person-centered, timely, efficient, and equitable” (5,6). Specifically, team-based care is recognized as an important innovation that is necessary for primary care clinics to adapt to the emerging needs of patients and respond to the external challenges of delivering patient-centered care (1,7-9).
The need for comprehensive, integrative service is especially acute for vulnerable patient populations with complex health needs and social barriers to care—those who are at a particularly greater risk for poor health care access and outcomes (10). Complex health needs entail overlapping preventive, chronic, and mental health needs (11-13) often coupled with social barriers to care including inadequate housing, food insecurity, and the lack of health insurance (14,15) which can create challenges to accessing essential and necessary care (16). As a result, individuals with high social barriers (e.g. , low-income, uninsured, and lacking a usual source of care) are more likely to miss or delay necessary health care services like primary care (17).
Prior work suggests that in order to address vulnerable populations’ physical, mental health, and social needs simultaneously in practice, primary care clinics will need to embrace teamwork (7) and team-based approaches (18,19). More specifically, this means having multiple types of care available and coordinated to treat more complex health and social needs of vulnerable populations (20). There is also an expectation that a variety of non-physician providers including but not limited to care managers, social workers, pharmacists, registered nurses, behavioral health specialists, and community health workers, will both deliver more preventative and chronic disease management services and help physicians implement patient care plans and patient education (9,21).
Despite efforts to spread team-based care to vulnerable populations and otherwise address individuals’ social barriers to care (22-24) and its theorized importance (7), we have a limited understanding of the structures and processes by which primary care clinics attempt to provide higher quality care that reduces the especially high risk of poor patient outcomes. Specifically, we know little about how primary care clinic teams work to address the complex health and social needs of vulnerable patients given the challenges these patients face and the unique needs they present to clinics and their provider teams. The focus of our research, therefore, was to address this gap and examine how primary care clinics serving predominantly vulnerable populations employed team-based care to anticipate and adapt to the complex needs of their patients. We wanted to learn, specifically how do physician and non-physician providers enact team-based care in clinics primarily serving vulnerable patients? That is, who is included in the care team, how do they work together, and, what strategies enable primary care teams to provide comprehensive care to largely complex and vulnerable patients? To answer these questions, we conducted interviews with a range of health care providers from seven primary care clinics to identify the structures and processes through which team-based, comprehensive care for vulnerable populations is delivered. We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/jhmhp-20-102).
Methods
Study sites and sampling approach
We examined primary care clinics participating in a population health management program for uninsured patients located in Virginia. As these vulnerable patients require greater care coordination, it was ideal to examine how team-based care was carried out in settings designed to manage this complexity. This strategy also allowed us to observe variation in how team-based care was delivered in different clinics for patients who had unique health and psychosocial needs. A total of 30 clinics were initially identified and seven responded to the first author’s request to participate. A program coordinator affiliated with the population health management program was instrumental in the facilitation of participant recruitment.
The first author initially used purposive sampling to recruit participants from multiple disciplines including medicine, nursing, behavioral health, social work, and pharmacy, however, due to logistical barriers, it became difficult to recruit sufficient participants for this study solely using purposive sampling. As a result, the first author also allowed research participants to identify potential recruits for interviews (i.e. , snowball sampling).
Data collection
The first author conducted one-on-one semi-structured interviews at the seven primary care clinics between July 2016 and March 2017. The purpose of these interviews was to elicit examples of how physicians and non-physician providers worked together to perform team-based primary care. The first author used a semi-structured interview protocol consisting of different questions asking participants to describe their team characteristics (e.g. , team composition) and the activities they engaged in with other providers to address the challenges related to delivering high-quality primary care in the clinic setting. The purpose of these interviews was to capture a broad range of perspectives relevant to the delivery of team-based primary care by asking participants to describe their experiences engaging in team activities and behaviors in the context of their clinic. The tenets of theoretical sampling guided the direction of the interviews (25): as initial themes emerged from earlier interviews, they shaped the focus of subsequent interviews. Thus, questions asked in subsequent interviews were tailored to capture more information on the categories that emerged during the analysis of preliminary interviews. The semi-structured interview protocol, therefore, was refined after an initial round of 12 interviews. Specifically, the initial 12 interviews focused on asking participants to describe how they felt speaking up or communicating patient-specific issues to other team members and the challenges associated with communicating these issues while the remaining 18 interviews focused on asking participants to describe how and when they reached-out to other team members or resources to help a patient (interview protocols are available upon request). All interviews were digitally recorded and transcribed verbatim. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Virginia Commonwealth University (IRB No. HM20005714) and informed consent was taken from all the participants.
Data analysis
Coding occurred in multiple stages following the constant comparative method (25). The first author initially performed open coding allowing for concepts and categories to develop based on the properties and dimensions of the text (26). Provisional codes were developed as the first author read and reread the transcripts. Provisional codes were used to capture actions, behaviors, and structures related to team-based care or clinic characteristics that seemed to facilitate or impede team-based care. As new provisional codes emerged, the transcripts were reanalyzed using the new coding structure. This process was used to analyze patterns in the coded data in order to integrate codes into theoretical categories. Throughout the analysis, memos were written to make connections between codes and the data and facilitate constant comparison (27). The first two co-authors met every 2 to 3 weeks to review the coding scheme and refine the research findings. The first author also used the following coding rule to keep coding consistent: at least two participants had to have described the same or similar phenomenon related to delivering team-based care. The two participants did not have to be from the same clinic or work together on the same team. This rule was used to enhance the validity of the coding process but also to identify themes that repeatedly emerged across interviews and clinics.
Results
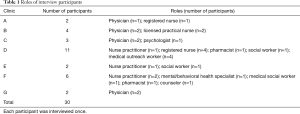
A total of 30 individuals participated in face-to-face interviews. Seventy percent of participants were female and 60 percent provided patient care full-time (i.e. , at least 5 days per week). At the time interviews were conducted, participants worked on average about five years in their respective roles. Table 1 summarizes the number of participants from each clinic and their corresponding roles as well, Table 2 contains a description of the seven participating clinics.
Full table

Full table
All seven clinics provided health services to predominantly poor patient populations (either Medicaid-insured or uninsured), used electronic medical records, and had access to behavioral and social health providers (e.g. , psychologists and social workers) on-site or on a referral basis. Five of the primary care clinics were owned and operated by an academic medical center, one was a free clinic, and one was a federally qualified health center (FQHC). Each clinic had implemented the use of case managers and other health care providers (e.g. , social work and community health workers) to support patients with chronic and severe medical conditions.
Three theoretical categories emerged from the data analysis—patient characteristics and complexity, using team huddles to anticipate patients’ needs, and mobilizing expertise through co-location and the use of warm-handoffs. The specific form of the patient characteristics and complexities necessitated strategies to address them that included huddles and handoffs. Next, we describe these themes in greater detail, including providing verbatim quotations that support our characterization of these categories.
Patient characteristics and complexity
Participants across all clinics gave rich descriptions of the vulnerable patients they typically came in contact with in their clinic, further motivating the need for teamwork and comprehensive approaches to care delivery. Participants described how these patients tended to have both medical and social needs that were difficult to manage all at once. One participant reflected (Psychologist, Clinic C), “And then you have people who are more complex, um, definitely with like a myriad of, mental health, and physical health all coming into a gigantic storm and they’re all playing off of one another. ”
Participants from some clinics were explicit in recognizing how providing necessary clinical care was made more difficult by a patient’s unmet social needs. Specifically, medical outreach workers (MOWs) and clinicians suggested that missing appointments was often a function of patients lacking basic material resources, like housing and transportation. For example, as one MOW explained (MOW, Clinic D), “Transportation is one of those things that prevents them from picking up their medications, from making their doctor’s appointments. Um, so transportation is always a very high need…just having resources for food and housing…So those are really big on the list. ”
Furthermore, participants understood that without addressing their patients’ more basic needs, it would be difficult to manage their health. The acknowledgment of vulnerable patients’ complex medical and social needs, however, did not always correspond with clinics being better able to anticipate and respond to them. Next, we describe the differences in how clinics used team huddles and mobilized care team members’ expertise to attempt to address vulnerable patients’ complex needs.
Strategies for addressing vulnerable patients’ complex needs
Our analysis revealed that primary care clinics used two major strategies to address vulnerable patients’ complex care needs: (I) using team huddles to anticipate patients’ needs and (II) mobilizing requisite expertise through co-location and warm-handoffs. Participants often described these strategies as being helpful in terms of delivering team-based primary care and providing high quality care and disease management for vulnerable patients.
Using team huddles to anticipate patients’ needs
Participants from Clinics C, D, and F described how daily huddles and team meetings were instrumental for developing a shared understanding of patients’ needs and team members’ particular roles in addressing those needs. Team members used these huddles to offer information about patients’ challenges accessing various community resources and identifying options to mitigate these barriers.
“So the purpose of the team huddles is to inform the team members what patient each team member needs to see and why, and also to find out are there any barriers of care that we need to troubleshoot from. And so [the nurse practitioner] leads the team huddles. We are open and honest, and we give (the nurse practitioner) our opinions. ” (MOW, Clinic D).
The use of huddles to share patient-specific information enabled team members to better identify which community resources or expertise would be necessary to address the patient’s medical issues or social barriers to care. As one mental health specialist reflected, “And the case manager can step in and say well let’s see what we can do about facilitating that through Meals on Wheels or something like that where [the patient] get their, they get some of their needs met better. We had some work done on coordinating with the YMCA or the, their diabetes program and getting the case managers to refer a lot of diabetic clients to them for exercise. Or diet, nutritional needs, and meeting their nutritional needs for education and things like that. ” (Mental Health Specialist, Clinic F).
A counselor from Clinic F also described how huddles and team meetings allowed them to understand how team members were working together to address their patients’ needs and ways they could better combine their skills to provide better patient care.
“I think by having our huddles or our team meeting, I get to hear other dimensions of the client that we’re all working with in conjunction. I get to hear the – the therapist, their perspective of the person that we see. I get to know exactly what the medical issues are… But it gives us the opportunity to learn from each other and we take all of our skills and kind of put them together, and I think that we provide a better service when we do that. ” (Counselor, Clinic F).
These team huddles also made team members aware about what they needed to do to follow up with a patient. By focusing conversations on specific patients that were particularly challenging to engage, team members could expose gaps in the patient’s care plan and it facilitated strategizing sessions on how to pre-emptively and proactively address the patient’s needs and better engage them with the team. Participants explained how they used huddles to coordinate team responsibilities and address care-related concerns efficiently by creating and using “huddle sheets” as a way to collect standardized information about patients’ health maintenance needs. For instance, worksheets were used to remind team members which patients needed to have certain blood tests performed during or before their upcoming clinical visit.
“Before each session, the physician and the nurse talk and the nurses have a worksheet that they’ve completed, which has very basic stuff about the patient, so their age, what they’re coming in for, and then the nurses do a brief chart review that looks at some of the health maintenance stuff. Then we talk together about okay, well I noticed that she was anemic on her last visit so let’s make sure we go ahead and get a hemoglobin when she comes in, you know, point of care tests, and we kind of do that kinda thing. ” (Physician, Clinic C).
However, there were clinics that used huddles in a less patient-focused manner. More general uses of huddles frustrated some members of the teams because they felt the huddles were a unique opportunity to focus on specific patients and represented a missed opportunity when they did not. For example, Clinic B used huddles to debrief staff on events that required clinician intervention and for addressing operational issues of the clinic. One nurse described how their clinic used huddles to discuss situations that posed a threat to patient safety or less serious situations that impacted patient flow (i.e. , efficiency) such as having insufficient supplies (Licensed Practical Nurse, Clinic B). Furthermore, a nurse practitioner from Clinic E expressed her dissatisfaction with the current way her team was using huddles. More specifically, their team huddles were used as a platform to share operational issues and general clinic reminders, not in-depth information about specific patients.
“What (the huddles) have—dare I say—disintegrated into, is kind of a more mundane thing – like we’ll say, ‘Everybody make sure you’re wearing your nametag. Make sure that when you park you’re really saving space in the back lot for the patients’… (Those announcements are) not really contributing to a culture of safety and quality”. (Nurse Practitioner, Clinic E).
Mobilizing requisite expertise through co-location and warm-handoffs
In the five clinics (C-G) where physician and non-physician providers shared the same workspace (i.e. , co-location), numerous participants described the advantages of having access to different types of clinical and non-clinical expertise to help address a variety of patient demands. The accessibility of non-physician expertise (e.g. , psychologists and social workers) enabled primary care teams to enact “warm handoffs”—or direct exchange of information and the transition of patient accountability from one team member to another. Warm handoffs were common in situations when patients demonstrated one or more educational deficiencies, behavioral health issues, and/or social support needs.
“(The patients) have nothing, they’re really, really sick…I feel like my responsibility for those other aspects are already solved by having resources…when you have a social worker, I don’t have to be a hero and try and track everything down…He can do eyeglasses…he can do other things that I don’t have to be an expert on…I could and I would do it, but it’s easier when you have some of those resources to be able to utilize them. ” (Pharmacist, Clinic D).
From participants’ perspectives, when warm handoffs were possible, it allowed other non-physician providers to establish a relationship with the patient so that they could start to identify some of the non-medical issues that were affecting the patient’s health.
“(The psychologists) sit back in the doctors’ workroom… it’s really easy to communicate with them… You’ll say, “Hey, I’ve got a patient here who’s feeling really down. Her brother died a week ago,” and at that point the psychologist will say, “Yeah, we have time to see them today,” and you kind of give a big of a handoff in terms of what’s going on… [The psychologist will] check with the patient… You’ll discuss what’s going on, and you’ll talk about like the psychologist will say, “I gave her… some coping mechanisms and diet guidelines or whatever. ” And I’ll say, “Okay, that sounds great,” or I’ll say, “What did you think about how she’s talking about blah, blah, blah?” Then they’ll give what they thought about that, and then I’ll coordinate with the psychologist, like a follow-up appointment…” (Physician, Clinic B).
Warm handoffs played an important role because they allowed physicians and non-physicians to see patients on the same day which meant patients could more easily access the necessary clinical services, counseling, or education to address their needs.
“…having the social worker literally in our office five days a week has resulted in warm handoffs and that is one of the best things…the first thing I do is say [to the patient], “Would you mind seeing Miss P. for me?” And I would walk her over and say, “Miss P. , do you think you could peek in on us in room six?” And I would literally hand them off and then (the social worker) would sit with the patient and figure things out. ” (Physician, Clinic C).
Also, in co-located clinics, team members could identify the appropriate team member(s) more easily which made it possible for providers to engage in cross-disciplinary collaboration more frequently.
“But as the provider may need something, it could be daily. It could be weekly. [The conversation] varies… we’re here on the same floor, so we have easy access to each other… I used to be [upstairs], so when we started integrating the team members, I [moved down a floor] so I could be touched and reached out. ” (Counselor, Clinic F).
Unlike the co-located clinics that routinely enacted warm handoffs to perform patient referrals, the clinical and non-clinical expertise available to primary care teams from Clinics A and B were more dispersed. In other words, these teams relied on standard referral processes, like paging or making phone calls to outside personnel, with the expectation that a team member would follow up with the patient. These standard, more traditional referral processes were enacted when the needs of the specific patient were outside the scope of the team’s expertise.
“Well for the social work case we have to request social work to come see a specific patient…after the fact where we say, “Well we will ask our social worker to contact you and see if there are resources in the community…that’s how that is handled. ” (Physician, Clinic A).
Because physicians and social workers in Clinics A and B did not always work in the same vicinity, physicians often could not present the patient to a social worker nor introduce the social worker as member of the patient’s care team.
Discussion
The complexity of vulnerable patients with unmet basic needs (e.g. , transportation, housing) necessitates holistic approaches to care delivery. In this study we explored how primary care clinics deployed team-based care strategies to address these patients’ medical and non-medical needs. In doing so, we move research forward by further illuminating the necessity of team-based care and specifying how it is used to address previously unmet needs of vulnerable individuals. Our analysis suggests that some primary care clinics were able to implement strategies to anticipate and address the needs of vulnerable patients through the use of huddles and warm handoffs. Study participants described how these strategies helped incorporate patients’ social barriers to care into treatment planning and allowed team members to coordinate care in order to address whole person needs. We also found evidence of differences across clinics with respect to how they use huddles and handoffs and how that reflects broader differences in capabilities to enlist and utilize the requisite expertise to address patients’ social barriers to care and often complex health needs.
Our research builds on studies (4,28-30) that previously recognized the importance of team-based primary care to address the needs of complex patients and for improving the delivery of primary care services. We reaffirm this idea by identifying two structures and processes that underpin what the team members perceive as effective team-based care. Specifically, we found that physician and non-physician providers rely on and use team huddles to develop proactive and holistic strategies for addressing the complex medical and social needs of vulnerable patients often with chronic conditions. In developing and executing these strategies, there is evidence that primary care teams differ with respect to how they use huddles and deploy their expertise to address patients’ needs. For example, when primary care teams have access to non-physician expertise to engage in warm handoffs, the face-to-face interactions between providers helps develop a shared understanding of individual and mutual responsibilities and the appropriate course of action more swiftly. For instance, the dialog between team members during warm handoffs brought to bear information about patients’ conditions that led to providers spelling out their specific next steps (e.g. , schedule a follow-up visit, provide a same-day appointment, or provide in-person counseling). The accessibility of non-physicians, like psychologists and social workers, made for more efficient information sharing and enabled teams to close the communication loop. In addition, warm handoffs provide a context and suggest a process that allows team members to build higher quality interpersonal relationships and better understand each other’s expertise (31).
Prior research (2,19,32-34) has demonstrated the benefits of teamwork for improving processes of care (e.g. , diabetes care, hypertension management) and reducing physician workload. Our research extends this work to how teams address patients’ complex, multi-faceted health care and social needs. Our research provides rich detail about how primary care teams proactively use huddles and warm handoffs to address vulnerable patients’ basic unmet health needs and the social (e.g. , financial, intrapersonal) barriers to effective treatment. For example, MOWs have been previously described to play an important role in connecting patients to a variety of community resources like counseling, preventative screenings, and social support services (35). In Clinic D the primary care team dedicated time during huddles to identify patients who could potentially benefit from these community resources. The MOWs coordinated with external partners and assisted specific patients connecting with these community organizations. However, some clinics systematically missed these opportunities by, for instance, using team huddles to discuss general clinic operations as opposed to particular patient needs. Interviewees reported that, consequently, there was a need to improve team coordination and better prepare for incoming patient visits. Furthermore, when expertise is not co-located, as was the case in some of our clinics (i.e. , Clinics A and B), it may limit the team’s ability to have richer face-to-face interactions that lead to shared accountability.
Although there are multiple benefits for managers and physician leaders to implement team huddles to facilitate team-based care, our analyses suggested that the key is in how they are used by team members. Huddles that focus on the needs of specific patients may encourage team members with unique expertise (e.g. , accessing social resources) to engage in strategizing and problem-solving. Similarly, huddles can potentially facilitate knowledge sharing and seeking between the different providers which can make it easier for team members to know who specializes in a specific domain (e.g. , insurance policy changes) and make use of their expertise (36). These types of huddles may enhance providers’ self-efficacy and willingness to further engage in cross-disciplinary collaboration. The potential spillover effects of positive huddle experiences on provider self-efficacy and willingness to engage in interdisciplinary collaboration and communication thus merits examination in future research. Also, the extent to which regular (e.g. , daily) huddles and how they are conducted affect a team’s adaptability to changing demands is worth further investigation. For example, future research could examine the ways primary care teams conduct huddles overtime and explore how it enables providers to react to emergent events (e.g. , staffing shortage, decline in a patient’s health status).
Practitioners and managers may also benefit from this research because it suggests some practical recommendations for sharpening and sustaining dialogue among members of interdisciplinary teams. Interpersonal processes such as knowledge-sharing can stimulate teams to combine their existing knowledge in novel ways and increase the team’s responsiveness to changes in patient demands (37). Our research adds the steps frontline providers can take to stimulate the sharing of expertise and knowledge by how they enact huddles or engage in warm handoffs. When these strategies are used to bridge disciplinary boundaries and marshal unique expertise as observed in our data, primary care team members are more likely to develop shared goals and shared understandings about roles and responsibilities. Future research could explore the relationship between these strategies and interpersonal processes like relational coordination (38). Also, in situations where team expertise is dispersed, providers may want to experiment with video conference applications as a way to initiate “virtual” handoffs if or when a patient requires a community resource. Such an approach may be particularly valuable for patients having limited technological skills, health literacy, or internet access to obtain these resources on their own.
Managers, providers, and patients could benefit from the development of the more nuanced strategies we identify in this research in order to fully consider and incorporate the social determinants of health essential to effectively serving vulnerable populations by including community expertise into how they deliver primary care. Consequently, leaders should be mindful of how to organize for integrating medical, behavioral, and social health providers. Table 3 offers recommendations that may assist leaders in implementing these strategies in practice.

Full table
Limitations
Our study has several limitations. First, team-based care was implemented at different times across clinics and it was difficult to pinpoint when each clinic formally implemented team-based care. Some teams had been in place for at least one year as a result of implementing the patient-centered medical home model (e.g. , Clinics D and F)—a specific type of care model that emphasizes the use of teams to provide comprehensive and coordinated care. Furthermore, in other clinics (e.g. , Clinics A and B), it was unclear whether team-based care was formally implemented and if it was implemented as part of a previous quality improvement initiative. Second, the findings are based on a relatively small number of clinics. This may limit the generalizability of our findings. We attempted to mitigate these concerns by examining a range of different types of clinics (i.e. , free clinic, FQHC, and varied academic medical center clinics) and did not observe systematic differences based on clinic type. Future research could further bolster our findings by using an even larger, more varied sample. On a related note, the strategies identified in this study may not translate to clinics serving less vulnerable populations. However, our research provides evidence that clinics should consider how primary care “looks” for different patient populations and not take a one-size-fits-all approach to how they provide health care services. Fourth, over a third of the participants for this study came from a single clinic (i.e. , Clinic D). As a result, our interpretation of the data around the perceptions of team huddles and warm hand-offs may have been skewed because several participants came from a single clinic within an academic medical center. Finally, as our study objective was exploratory in nature, our data did not allow us to test more formally whether the strategies we identified actually address patients’ unmet needs. For instance, researchers may want to explicitly test the relationship between the content of huddles (e.g. , expansively discussing the patient’s needs, planning for the visit) and patient referrals to and engagement with community resources as well as clinical outcomes.
Conclusions
As team-based primary care proliferates, managers, providers, and patients could potentially benefit from adopting and using team huddles to anticipate patients’ needs and mobilizing team expertise through the use of warm handoffs. When managing patients with complex health and social needs, clinics may especially benefit from deploying these structures and processes that more fully incorporates non-clinical expertise into how they deliver primary care.
Acknowledgments
The authors are grateful for the volunteers who participated in this study. Without them this research would not have been possible.
Funding: This publication resulted from Dr. DePuccio’s dissertation research for which funding was provided by the Virginia Commonwealth University Department of Health Administration.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Naleef Fareed, Ann Scheck McAlearney, and Susan D Moffatt-Bruce) for the series “Innovations and Practices that Influence Patient-Centered Health Care Delivery” published in Journal of Hospital Management and Health Policy. The article has undergone external peer review.
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/jhmhp-20-102
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jhmhp-20-102
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp-20-102). The series “Innovations and Practices that Influence Patient-Centered Health Care Delivery” was commissioned by the editorial office without any funding or sponsorship. SJS serves as an unpaid editorial board member of Journal of Hospital Management and Health Policy. MJD reports he received a dissertation award from the Virginia Commonwealth University, Department of Health Administration which supported data collection and analysis for this study. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Virginia Commonwealth University (IRB No. HM20005714) and informed consent was taken from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ghorob A, Bodenheimer T. Building teams in primary care: a practical guide. Fam Syst Health 2015;33:182-92. [Crossref] [PubMed]
- O’Malley AS, Gourevitch R, Draper K, et al. Overcoming challenges to teamwork in patient-centered medical homes: a qualitative study. J Gen Intern Med 2015;30:183-92. [Crossref] [PubMed]
- Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med 2008;21:427-40. [Crossref] [PubMed]
- Song H, Chien AT, Fisher J, et al. Development and validation of the primary care team dynamics survey. Health Serv Res 2015;50:897-921. [Crossref] [PubMed]
- Mitchell P, Wynia M, Golden R, et al. Core principles & values of effective team-based health care. Washington, DC: Institute of Medicine, 2012.
- Naylor MD, Coburn KD, Kurtzman ET, et al. Inter-professional team-based primary care for chronically ill adults: state of the science. ABIM Foundation Meeting to Advance Team-Based Care for the Chronically Ill in Ambulatory Settings. Philadelphia, 2010.
- Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA 2004;291:1246-51. [Crossref] [PubMed]
- Hochman M, Asch SM. Disruptive models in primary care: caring for high-needs, high-cost populations. J Gen Intern Med 2017;32:392-7. [Crossref] [PubMed]
- Hong CS, Siegel AL, Ferris TG. Caring for high-need, high-cost patients: what makes for a successful care management program? Issue Brief (Commonw Fund) 2014;19:1-19. [Crossref] [PubMed]
- Aday LA. At risk in America: the health and health care needs of vulnerable populations in the United States. San Francisco, CA: John Wiley & Sons, 2002.
- Bolen SD, Sage P, Perzynski AT, et al. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev 2016;17:18-32. [Crossref] [PubMed]
- Bolen SD, Stange KC. Investing in relationships and teams to support managing complexity. J Gen Intern Med 2017;32:241-2. [Crossref] [PubMed]
- Pass LE, Kennelty K, Carter BL. Self-identified barriers to rural mental health services in Iowa by older adults with multiple comorbidities: qualitative interview study. BMJ Open 2019;9:e029976. [Crossref] [PubMed]
- Palmer RC, Ismond D, Rodriquez EJ, et al. Social determinants of health: future directions for health disparities research. Am J Public Health 2019;109:S70-1. [Crossref] [PubMed]
- Centers for Disease Control and Prevention. Social Determinants of Health: Know What Affects Health. 2020. Available online: https://www.cdc.gov/socialdeterminants/index.htm
- Marmot M. Social determinants of health inequalities. Lancet 2005;365:1099-104. [Crossref] [PubMed]
- Shi L, Stevens GD. Vulnerability and unmet health care needs. The influence of multiple risk factors. J Gen Intern Med 2005;20:148-54. [Crossref] [PubMed]
- Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med 2009;169:1996-2002. [Crossref] [PubMed]
- Kennelty KA, Polgreen LA, Carter BL. Team-based care with pharmacists to improve blood pressure: a review of recent literature. Curr Hypertens Rep 2018;20:1. [Crossref] [PubMed]
- Kerrissey M, Satterstrom P, Leydon N, et al. Integrating: a managerial practice that enables implementation in fragmented health care environments. Health Care Manage Rev 2017;42:213-25. [Crossref] [PubMed]
- Hopley C, Andrews E, Klem P, et al. Evaluating the feasibility of a pharmacist-guided patient-driven intervention to improve blood pressure control in patients with CKD. Pilot Feasibility Stud 2019;5:23. [Crossref] [PubMed]
- Berry CA, Mijanovich T, Albert S, et al. Patient-centered medical home among small urban practices serving low-income and disadvantaged patients. Ann Fam Med 2013;11:S82-9. [Crossref] [PubMed]
- Garg A, Jack B, Zuckerman B. Addressing the social determinants of health within the patient-centered medical home: lessons from pediatrics. JAMA 2013;309:2001-2. [Crossref] [PubMed]
- Takach M. About half of the states are implementing patient-centered medical homes for their Medicaid populations. Health Aff (Millwood) 2012;31:2432-40. [Crossref] [PubMed]
- Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. New York: Aldine, 1967.
- Miles M, Huberman M. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, CA: Sage, 1994.
- Glaser BG. The constant comparative method of qualitative analysis. Soc Probl 1965;12:436-45. [Crossref]
- Giannitrapani KF, Glassman PA, Vang D, et al. Expanding the role of clinical pharmacists on interdisciplinary primary care teams for chronic pain and opioid management. BMC Fam Pract 2018;19:107. [Crossref] [PubMed]
- Meyers DJ, Chien AT, Nguyen KH, et al. Association of team-based primary care with health care utilization and costs among chronically ill patients. JAMA Intern Med 2019;179:54-61. [Crossref] [PubMed]
- Reiss-Brennan B, Brunisholz KD, Dredge C, et al. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 2016;316:826-34. [Crossref] [PubMed]
- Feldman MS, Rafaeli A. Organizational routines as sources of connections and understandings. J Manage Stud 2002;39:309-31. [Crossref]
- Benzer JK, Mohr DC, Evans L, et al. Team process variation across diabetes quality of care trajectories. Med Care Res Rev 2016;73:565-89. [Crossref] [PubMed]
- Sinsky CA, Bodenheimer T. Powering-up primary care teams: advanced team care with in-room support. Ann Fam Med 2019;17:367-71. [Crossref] [PubMed]
- Wagner EH, Flinter M, Hsu C, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract 2017;18:13. [Crossref] [PubMed]
- Thompson-Lastad A, Yen IH, Fleming MD, et al. Defining trauma in complex care management: safety-net providers’ perspectives on structural vulnerability and time. Soc Sci Med 2017;186:104-12. [Crossref] [PubMed]
- Goldenhar LM, Brady PW, Sutcliffe KM, et al. Huddling for high reliability and situation awareness. BMJ Qual Saf 2013;22:899-906. [Crossref] [PubMed]
- Safran DG, Miller W, Beckman H. Organizational dimensions of relationship-centered care. Theory, evidence, and practice. J Gen Intern Med 2006;21:S9-15. [Crossref] [PubMed]
- Hoffer Gittell J. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manage Sci 2002;48:1408-26. [Crossref]
Cite this article as: DePuccio MJ, McClelland LE, Vogus TJ, Mittler JN, Singer SJ. Team strategies to manage vulnerable patients’ complex health and social needs: considerations for implementing team-based primary care. J Hosp Manag Health Policy 2021;5:4.

