The creation of a certified palliative care program in a community hospital through education
Introduction
A Palliative Care Team (PCT) Initiative began in 2009 at a 182-bed community hospital located in the mid-Atlantic. In 2013, four years later, it was the 29th hospital and the first community hospital palliative care program to receive advanced certification by The Joint Commission (TJC) (1). This hospital is a part of a not-for-profit healthcare system based in Northern Virginia serving more than 2 million people each year. The system includes five hospitals which house just under 1,800 licensed hospital beds and in 2015 had close to 98,000 inpatient admissions. The desired outcome of the PCT initiative was to create an atmosphere of acceptance of a palliative care program as an integral part of health care through a culture change. This change in culture was propelled by structured educational programs anticipated to expand and augment knowledge of clinical and medical providers encouraging employment of a palliative care interdisciplinary consultation model. The result was expected to be an improvement in patient symptom management.
There is a difference between implementing or developing a palliative care program and implementing one that receives advanced certification in palliative care from TJC. To obtain the initial and subsequent certifications the program must meet and continue to meet the standards set by TJC that demonstrate consistently providing a very high quality of care to persons with serious illnesses. According to TJC, the standards are ‘state-of-the-art … expectations for organization performance that are reasonable, achievable and surveyable’ (2).
The article describes the process of preparing for implementation and certification of the PCT in a small community hospital. This includes how the PCT was developed, implemented, and how the hospital moved towards the culture change—the enculturation of the palliative care program. This is followed by the findings of a study, undertaken to evaluate the education for integration and enculturation of the palliative care program within the hospital over the course of first 3 years.
In 2009 one palliative trained physician began seeing patients in the intensive care unit (ICU) at the hospital. Over time the intensivists requested palliative participation at multidisciplinary morning rounds. The intensivists reported to medical staff and administration that their patients benefitted from the interdisciplinary collaboration and recommendations from the palliative viewpoint.
Continuation of the morning palliative rounding collaboration between 2009 and 2012 was sustained as the intensivists reported an increase in their satisfaction with patient care, resulting in discussions with senior hospital leadership to initiate a PCT. In early 2012 the senior leadership lent support to the development of a PCT. Initial goals were an improvement of the quality of patient care and to achieve Disease-Specific Certification for Advanced Palliative Care from TJC. Support was demonstrated with the provision to fund a palliative nurse (program coordinator), and later a social worker, and chaplain based on TJC (3) and the Center to Advance Palliative Care (CAPC) (4) recommendations for successful PCTs.
Growing a palliative care program in a community hospital, even with the guidance furnished by CAPC and TJC (3,4), had unique challenges. Some challenges are likely faced by other hospitals. The unique challenge was the difference of the institutional characteristics of the hospital compared to most hospitals that had or were developing a palliative care program. Hospitals with over 300 beds were seven times more likely to have a palliative care program than smaller hospitals. The hospital institutional characteristics that are associated with having palliative care programs have an accredited residency training program, association with a medical school, affiliation with the Catholic Church, and/or owning a hospice program, none of which are characteristics of the hospital. An important similarity was that the hospital had a cancer program approved by the American College of Surgery. Other similar characteristics were the non-profit status in a geographic area with a high percentage of residents having a college degree (5). Though Dumanovsky et al. (5) gathered data from 2,393 hospitals with 1,591 reporting having a palliative program, there was no data collected on how many had gone through the process of becoming certified and remaining certified for advanced palliative care.
Challenges that were likely common to many hospitals developing a palliative care program are the perceptions held by some of the medical staff, such as non-ICU physicians and nurses, and in the surrounding community. A common concern is that the PCT would “steal” patients, rather than collaborate to provide the highest quality care and coordinate transitions of care. Further, it has been reported that Primary Care Providers (PCPs) reject palliative care as they often focus on the cure of the disease at all costs (6-8). Many PCPs believed they were already delivering primary palliative care to their patients but did not have a complete understanding of all the specific benefits and burdens as related to options of care and the various integrative treatments provided by the PCT (7,8).
PCT Initiative
Program development
The plan to develop and implement a PCT was based on the framework of care required by TJC (3) to demonstrate exceptional patient and family-centered care, optimizing the quality of life for adult patients with serious illness. One of the first steps was soliciting opinions from a Palliative Advisory Board composed of representatives from each of the clinical and medical specialties within the hospital. This group was instrumental in conceptualizing the development plan goals. Improvement pathways toward enhanced quality of life were directed through:
- The creation of a palliative care program, led by a specially trained interdisciplinary team;
- Allocating time devoted to intensive family meetings, incorporating patient/family counseling;
- Ensuring the inclusion of the patient and family (anyone so designated by the patient) as members of the team;
- Integration of palliative care with curative treatment as standard patient care;
- Using evidence-based national guidelines in the development of processes resulting in clear pathways to support patient care.
The model selected was interdisciplinary consultation, such that PCT members would be consultants to the medical staff. According to Kelley and Morrison (9), this is the most common and successful model of hospital palliative care. Further, it would meet the overall goal of improved care for patients and families. The initial plan was for a consult to be initiated when a physician made a direct referral. A major objective was that over time screening would be conducted by clinical staff to identify appropriate patients and contact the physician rather than waiting for a referral. Thus a modification was made to the electronic health record (EHR) to allow for efficient screening and enhance communication among the interdisciplinary team.
Another step towards the successful implementation of the PCT was to enlist the cooperation and support from community palliative and hospice providers with hospital privileges (physicians and advanced practice nurses) to use the interdisciplinary consultation model of Palliative Care. This was necessary to meet one of TJC (3) requirements requiring 24/7 coverage of palliative care either in-house or on-call.
Education—formal and informal
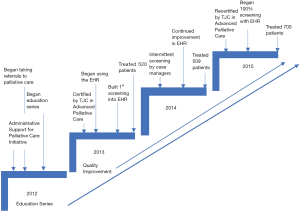
To meet these goals the PCT planned to engage the healthcare providers in the hospital and in the community, through education and identification of champions across health care disciplines (such as administration, medical staff, and nursing). Figure 1 shows the timeline of the developing and implementation of the PCI from 2012 to 2015.
Specifically, the program coordinator developed and implemented various levels of education to be delivered formally and informally. Examples of informal education include agenda slated case studies at departmental meetings and Tumor Boards, hallway encounters and elevators, group “safety huddles”. These opportunities included discussions about Advance Directive, Physician Orders for Scope of Treatment (POST), and the difference between palliative care, hospice, and comfort care. An example of the formal education was conventional continuing medical education (CME, CNE) offerings. Further, four nurses from strategic areas in the hospital (ICU, oncology, ED, and medicine) completed the End-of-Life Nursing Consortium (ELNEC) Train-the-trainers program. This allowed these nurses to educate their colleagues and offer support, in both formal and informal settings. The use of champions, professionals with established buy-in, provided peer-to-peer consultation on how the PCT helped their patients, another informal method.
The conventional educational opportunities, using a dyadic format, presented content on how the PCT could improve the quality of patient care, support providers and staff in their practices, improve the satisfaction of the patient and family members with hospital services, and improve the quality of life. The education was tailored to specialties, such as support for Case Management, addressing dietary needs and palliative care, and the need for physiotherapy and occupational therapy to improve quality of life and reduce fatigue. Physiotherapists and occupational therapists attended these trainings. As well as attending the formal educational opportunities nurses and social workers were also provided training outlining palliative and hospice care and their differences. Disease-specific options of care were explored to increase comprehension of the palliative approach to goals of care conversations. Over time both the medical and non-medical community requested training on how to have “difficult conversations”. The development of additional educational opportunities for the general community expanded the outreach of the program. Table 1 provides an outline of the dyadic educational program topics and examples.
Table 1
| Topic | Example |
|---|---|
| Introduction to palliative care and hospice | Definition and history of palliative care; definition and history of hospice |
| Survivorship with family and patient support through palliative care | Definition and difference between palliative care and hospice; “Every day you are alive, you are a survivor”; self-care: meditation, yoga, and guided imagery |
| Guidelines for Inpatient Palliative Care Model | Best practice model; plans for using the model; incorporating palliative care into clinical practice |
| Cultural diversity | Communication styles; locus of decision making |
| Grieving and bereavement | What grief is; what grief may look like; bereavement resources |
| Identifying and screening patients | Which patients would benefit from including the PCT? |
| Implementation and skill-building | Facilitate identification of personal attitudes and needs |
| Appraising the patient and family | Opening the door to deep conversation; identifying evidence of need; difficult conversations |
| Advance care planning | Living wills; power of attorney medical; 5 Wishes; national POLST paradigm |
| Options of care | What patients and caregivers need to know; disease specific benefits and burdens of care; other available services (i.e., music, Reiki, meditation, legacy work) |
| Comfort care | What is it really |
| Self-care for clinicians | Meditation; yoga; healthy diet; debriefing |
| Program success and improvements | Identify methods to improve care; how changes can be evaluated |
| Strategies and wrap-up | Barriers and facilitators to implementation of palliative care in a hospital setting |
The formal education was offered more than once and at different times and focused on specific disciplines. Offering the training at different times during the day allowed access to the training by all healthcare providers and staff regardless of the shift they worked. The informal education was available anytime during the day and not just during a 9 to 5 time frame from the program coordinator. With the use of ELNEC trainers and champions, informal education was available when another health provider had a question. It was also offered whenever a trainer or champion thought the time was right to provide additional guidance about palliative care for a specific care.
Specific aims of the initiative
In parallel with providing education program, the specific aims of this initiative were set forth and approved by the administration. These aims were to:
- Establish a standard approach for palliative care services:
- Standardize education;
- Develop a dashboard for operational, productivity, and clinical outcomes;
- Expand education.
- Reduce the time to obtain Palliative consults;
- Improve the quality and efficiency of palliative care delivery to:
- Reduce hospital length of stay (LOS) with early consultation;
- Reduce 30-day readmissions using education, establishing informed goals of care;
- Facilitate patients/families to identify personal goals with POST, which is a part of the national physician orders for life sustaining treatment (POLST) paradigm;
- To create health system strategies to:
- Improve care transitions;
- Integrate palliative care to community and healthcare settings.
To evaluate the implementation of the initiative retrospective data on all patients referred to and treated by the PCT during the first 3 years of certification were utilized. The primary purpose was to explore if the data indicated that development and implementation of the PCT resulted in a tangible change of hospital culture regarding the use of the PCT. Secondarily, exploring whether completing Aim 1—to establish a standard approach for Palliative care services—demonstrated improvement in Aim4b—integrate palliative care to community and healthcare settings.
Methods
Design
This secondary analysis study of clinical data previously collected on patients treated by the PCT was based on the following data: demographics, hospitalization data, and palliative care information (Table 2). This study was approved by the IRBs at the Inova Healthcare System (15.2129) and The Catholic University of America (No. 16-008).
Table 2
| Demographic | Hospitalization | Palliative care |
|---|---|---|
| Sex | Level of care | Pain scores |
| Age | LOS | Primary diagnosis for PC |
| Race | LACE | – |
| Ethnicity | Acuity | – |
| Marital status | Discharge unit | – |
| Deposition at discharge |
LOS, length of stay; LACE, LACE Index Scoring Tool for Risk Assessment of Hospital Readmission; PC, palliative care.
Data and sample
Retrospective data was extracted from the EHR on all patients seen by the PCT. Both the EHR and the PCT were concurrent ventures resulting in both programs evolving simultaneously. The outcome of this was that PCT data requests for changes in the EHR often experienced delays in implementation due to the high volume of requests for changes from the whole system. Identification of additional data points for collection increased over this period as an outcome of continuous quality improvement measures, a requirement of certification. With these obstacles and changes comparisons across all three years was not always possible.
Inclusion criteria were: over the age of 18, had a palliative care referral, and were admitted between January 1, 2013 and December 31, 2015. Those patients that had a referral but were not hospitalized or had a stay of 24 hours or less were not included in the final dataset. This resulted in a sample size of 1,408.
Demographic data
As noted in Table 1 the demographic data used in this study included: sex, race, ethnicity, marital status, and age. All ages reported as 90 or older were combined into the age of 89 for this analysis.
Hospitalization data
- Level of care based on history, examination, and medical decision-making (E & M):
- Used for billing purposes (10).
- LOS:
- Total hospitalization;
- LOS before PCT referral.
- LACE Index Scoring Tool For Risk Assessment for Hospital Readmission or Emergency Department (ED) visits:
- Index includes LOS (L), acuity (A), comorbidities (C), and ED visits (E);
- Scores range from 0 to 19;
- A score of 10 or higher interpreted as high risk for readmission or use of ED post discharge (11).
- Acuity was the severity of the patient’s medical problem, and the number of resources likely needed to stabilize the patient:
- The acuity score is calculated using the Emergency Severity Index (ESI), a five-item algorithm;
- Scores range from 1 (high, in need of immediate, life-saving interventions) to 5 (non-urgent) (12).
- Discharge unit was the hospital location of the patient on the day of discharge (general medicine, Telemetry, or ICU).
- Disposition identifies the locale where the patient transitioned, including expired (patient died in the hospital), home (with or without homecare support), hospice (either home or inpatient), or other institutions (such as short-term nursing facility or inpatient rehabilitation).
Palliative care data
- Pain scores documented at three points in time:
- Admission to PC;
- 48 hours later;
- Within the last 24 hours of hospitalization;
- Pain scores ranged from 0 (no pain) to 10 (worst imaginable pain). A score of 4 is the cutoff point for undertreated pain;
- Primary PC diagnosis identified the underlying diagnosis that resulted in symptoms leading to the patient’s admission.
Analysis plan
The analysis plan was to present univariate analysis on all the variables, for analysis of difference or relationships chi-square, independent t-test, ANOVA’s, and Pearson’s correlations were to be used. If the data had significant variance independent samples median tests were to be used.
Results
Demographics
Over the 3 years most of the palliative care patients were female (58.5%, 55.0%, and 58.1%, respectively), white (74.9%, 69.3%, and 72.9%, respectively), a clear majority were non-Hispanic or Latino (89.6%, 91.5%, and 93.6%, respectively), and married (43.0%, 51.5%, and 46.8%, respectively). The mean ages over the 3 years were 75.3, 73.2, and 72.2, respectively (Table 2). The only significant finding was that over the three years the number of non-Hispanic or Latino patients increased over the 3 years (χ2=75.19, P<0.001) (Table 3).
Table 3
| Characteristics | 2013 (n=443) | 2014 (n=407) | 2015 (n=558) | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Sex | ||||||||
| Male | 184 | 41.5 | 183 | 45.0 | 234 | 41.9 | ||
| Female | 259 | 58.5 | 224 | 55.0 | 324 | 58.1 | ||
| Race | ||||||||
| White or Caucasian | 314 | 74.9 | 269 | 69.3 | 388 | 72.9 | ||
| Non-white/other | 105 | 25.1 | 119 | 30.7 | 144 | 30.7 | ||
| Ethnicity* | ||||||||
| Non-Hispanic or Latino | 266 | 89.6 | 335 | 91.5 | 508 | 93.6 | ||
| Hispanic or Latino | 15 | 5.3 | 22 | 6.2 | 28 | 5.2 | ||
| Marital status | ||||||||
| Single | 58 | 13.1 | 57 | 14.2 | 87 | 15.7 | ||
| Married/significant other | 186 | 43.0 | 206 | 51.5 | 259 | 46.8 | ||
| Divorced/separated | 38 | 8.6 | 29 | 7.2 | 42 | 7.6 | ||
| Widowed | 151 | 34.9 | 108 | 27.0 | 165 | 29.8 | ||
| Age (all over 90 collapsed into 89) | 75.3 (14.9)# | 67–88§ | 73.2 (15.5)# | 64–86§ | 72.2 (16.7)# | 62–87§ | ||
* indicates P<0.05; # indicates data of mean (SD); § indicates data of IQ range.
Hospitalization data
There was a statistically significant change in the percentage of patients at the various levels of care (χ2=27.46, P<0.001) on admission. This was found between year 2 and 3 with a significant increase in patients at level 4 on admission. A statistically significant change in discharge unit was seen over the three years. It was more likely that a patient would be discharged from the general medicine unit in year two (53.3%) than in year one (45.6%) and in year one more likely to be discharged from a telemetry unit (44.5%) than in years two and three (34.2%, 36.9%, respectively) (χ2=12.13, P<0.05). Overall there was a statistically significant change in the proportion of patients discharged (excluding those who died inpatient) to hospice and home (χ2=26.8, P<0.001). During years one and two patients were more likely to be discharged to a hospice (55.6%, 50.7%, respectively) and in year three they were more likely to be discharged home (53.4%). Regarding those who died while in the hospital, the percentages were consistent at 16.6%, 18.9% and 16.3%. (Table 4)
Table 4
| Characteristics | 2013 | 2014 | 2015 | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Level of care* | ||||||||
| Level 3 | 6 | 2.0 | 9 | 2.4 | 14 | 2.7 | ||
| Level 4 | 96 | 32.1 | 132 | 34.6a | 251 | 47.8a | ||
| Level 5 | 184 | 61.5 | 226 | 59.2 | 242 | 46.1 | ||
| Critical care | 13 | 4.3 | 15 | 3.9 | 18 | 3.4 | ||
| Discharge unit* | ||||||||
| ICU | 44 | 9.9 | 51 | 12.5 | 54 | 9.7 | ||
| General medicine | 202 | 45.6a | 217 | 53.3a | 298 | 53.4 | ||
| Cardiac | 139 | 44.5a,b | 392 | 34.2a | 206 | 36.9b | ||
| Discharge disposition* | ||||||||
| Home (w/wo home care) | 131 | 31.5a | 122 | 33.4b | 236 | 44.7a,b | ||
| Hospice (home/medical) | 193 | 46.4a,b | 150 | 41.1a | 168 | 31.8b | ||
| Institution (SNF, rehab, assisted living) | 23 | 5.5 | 24 | 6.6 | 38 | 7.2 | ||
| Expired | 69 | 16.6 | 69 | 18.9 | 86 | 16.3 | ||
| Total LOS (0 means died day of admission) | 8.0 (6.0)# | 1–37§ | 7.9(6.2)# | 1–45§ | 7.5 (5.9)# | 1–48§ | ||
| LOS prior to PC | – | – | 3.8 (3.9)# | 1–24§ | 3.3 (3.0)# | 1–17§ | ||
| LACE score* | 8.3 (3.2)# | 1–19§ | 9.4 (2.6)# | 4–17§ | 10.3(3.3)# | 1–18§ | ||
| Acuity score | 2.4 (0.6)# | 1–4§ | 2.5 (0.5)# | 1–4§ | 2.5(0.6)# | 1–5§ | ||
*, Statistically significant finding in the variable; # indicates data of mean (SD); § indicates data of range; a,b,c, designation of significant finding between years. ICU, intensive care unit; LOS, length of stay; LACE, LACE Index Scoring Tool for Risk Assessment of Hospital Readmission; PC, palliative care.
The mean total LOS decreased over the 3 years were 8.0, 7.9, and 7.5. The mean LOS before referral (no data available for year 1) declined from year 2 (3.8 days) to year 3 (3.4 days). The mean acuity scores remained consistent (2.4, 2.5, and 2.5) over the time period. None of these changes were statistically significant. The mean LACE score was statistically significantly different over the 3 years (H2=36.56, P<0.001) which increased each year from 8.3 to 9.4 to 10.3.
Palliative care data (only available for year 3)
Pain
With the implementation of a new EHR, the retrieval of pain scores was impacted even though the pain scores were documented it was not automatically retrieved via a computerized report. Therefore, just under 55% (n=306) of data was able to be retrieved. Of these 97 (21.7%) reported a pain score of 4 or greater. At time 2, 48 hours after admission, 55% (n=307) of the sample had recorded pain scores and of these 111 (36.2%) reported undertreated pain. For the last pain score, the percent of patients with a pain score was just under 100% (n=556), and 100 (18.0%) reported undertreated pain. Ninety-seven of the patients had pain scores at each data point. The boxplots show the distribution of the pain scores of 4 or greater at each time point during year 3 (Chart 1).
There were no significant differences in pain score at any of the three points for level of care at admission or diagnosis. During year 3 there were statistically significant relationships between acuity and the first pain score (r=0.148, P<0.05), the pain score at 48 hours (r=0.187, P<0.01), and the last pain score (r=0.093, P<0.05). Acuity explains a small proportion of the variance at each time, 2%, 3.5%, and less than 1%, respectively. The sicker the patient, the more likely they were to have lower pain scores.
Primary diagnosis for palliative care
The underlying primary diagnoses that were used to help identify the need for palliative care were documented for 368 (66%) patients admitted in year 3, of these 81.5% had a Cancer, Cardiac, Pulmonary, Sepsis/Infectious Disease, or Neurological diagnosis. The remaining diagnoses in the year 3 sample were Gastrointestinal, Pain, Nephrology, or other (Table 5).
Table 5
| Diagnosis | N | % |
|---|---|---|
| Cancer | 98 | 26.6 |
| Cardiac | 57 | 15.5 |
| Pulmonary | 55 | 14.9 |
| Sepsis/infections disease | 50 | 13.6 |
| Neurology | 40 | 10.9 |
| GI | 24 | 6.5 |
| Pain | 21 | 5.7 |
| Nephrology | 9 | 2.4 |
| Other | 14 | 3.8 |
Using the diagnoses that made up the 81.5% ANOVA’s were used to explore difference by the interval level demographic, hospital, and palliative care variables. There were statistically significant differences in mean age by diagnosis (F=14.56, P<0.001) and mean acuity (F=3.54, P<0.01). Those diagnosed with cancer were, on average, younger (68.7) than the other four diagnoses (mean ages =82.6, 76.4, 78.2, and 80.6, respectively). There was a statistically significant difference in mean acuity by diagnosis, this was found between pulmonary (mean =2.2) and cancer (mean =2.6). Those patients with a diagnosis of pulmonary disease when admitted were less ill than those diagnosed with cancer.
There was a statistically significant association between diagnosis and level of care at admission (χ2=22.8, P<0.05). Those patients diagnosed with cancer were more likely to be admitted as Level 4 (53.7%) while those patients with one of the other four diagnoses were more likely to be admitted as Level 5 (53.6%, 61.1%, 66.7%, 55%, respectively). There was a statistically significant association between discharge disposition and primary diagnosis (χ2=26.2, P<0.05). Of the patients that had a primary illness the diagnostic group that was most likely to die while in the hospital with palliative care were those with pulmonary disease (30%) and sepsis/infectious disease (31.9%). Those with cancer were discharged to home more often than any other group (50%) while those with cardiac or neurologic diseases were discharged to hospice (50% for both). There was a statistically significant association between the last pain score and primary diagnosis (χ2=12.5, P<0.05). Those diagnosed with cancer had a higher percentage of having a score of 4 or above (40.7%) as compared to cardiac, pulmonary, sepsis/infectious disease, and neurology (20.4%, 19.5%, 24.3%, and 11.8%).
Discussion
Referrals of patients to the PCT changed in the 3 years following certification. Years 1 and 2 had about the same number of patients, at 520 and 509, respectively, with over a 37% increase to 700 in year 3. The increase in the percentage of patients being seen with the level of care 4 and a decrease in the level of care 5, along with annually reduced age, suggests that patients were being referred closer to diagnosis. The decrease in discharges to hospice and an increase of discharges home indicated earlier disease trajectory consults. The decrease in the percentage of patients being discharged from the telemetry unit and increase from general medicine further suggests the effects of identifying goals of care. Another potential indicator of enculturation was the decrease in mean LOS between admission and referral.
The change in the pain scores over three-time points showed that at time 2 (48 hours after admission) the median undertreated pain was higher than at admission. It is expected for pain scores to increase in the first 48 to 60 hours as the PCT begins to adjust medications to use the fewest possible for the greatest benefit. For the patients in year 3 that had a primary diagnosis assigned there were differences regarding age, acuity, level of care at admission, discharge disposition, and pain levels at discharge. These findings are not surprising as these five diagnoses have different age at onset and trajectory. This information may be helpful in education for medical staffs, patients, and families.
Looking specifically at the PCT aims between 2012, when the leadership supported the establishment of the PCT, to the end of 2015 a standard approach to care had been developed. The staffing levels were determined. The education for the hospital staff and the community was developed and continually being offered. The data sets determined important for the operational, productivity, and clinical outcomes were identified. The improvement in data collection in other words missing data decreased substantially over the first 3 years of the program. The study provides support for the program’s success in the enculturation of the hospital and the community.
Limitations
The major source of limitations in this study was related to the parallel development of the EHR and the PCT. The data needs of the PCT evolved at the same time as the EHR was being incorporated as the portal for documentation and data collection for the hospital. An example is the new data points requested by the PCT in year 3 thus the data was not available in years 1 and 2. A second limitation was related to collecting PCT specific data and entering it into the new EHR which improved over the course of the 3 years.
Another limitation was that this study was done at only one community hospital in a large health system. This limitation was done intentionally to present how a PCT was developed and became successful in a community hospital.
Conclusions
The initiation and development of a certified advanced palliative care program at a community hospital required an interdisciplinary approach with leadership support to advance a culture change. As a result of this endeavor, there has been a marked change in workflow processes and outcome metrics.
This organizational experience provides lessons learned from successes and challenges, for other organizations embarking on this journey. The program is now being expanded system wide. Discussions around PCT inclusion in changing the culture of the whole health system through education at every level of hospital clinical and medical staffing continue to be encouraged.
The upsurge in acceptance of palliative care and escalation of patient referrals was interpreted to demonstrate both acceptance and approval of the supportive care. The decrease in LOS and readmission patterns illustrated the success of the team approach. Leaders of the team linked transformation in patient care to the perception that standardized education for all medical and clinical staff using evidenced based guidelines to develop and streamline processes had positive consequences.
The provision of compassionate, timely palliative care is essential to support quality of life and enhance the appropriate care delivery. While a disease may not be cured, a person with a disease can benefit from care that seeks to decrease suffering, and the family can benefit from support in caring for their loved one.
Acknowledgments
Thanks to Mary Ann Friesen, PhD, RN, CPHQ for her help in staying focused, editing, and helping move the manuscript through the health system.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jhmhp.2018.01.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the IRBs at the Inova Healthcare System (15.2129) and The Catholic University of America (No. 16-008). Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- INOVA Fair Oaks Hospital. 2013 Inova Fair Oaks Hospital Quality Report. Available online: https://www.inova.org/upload/docs/quality/ifoh-2013-quality-report.pdf
- The Joint Commission. Facts about joint commission standards. Available online: https://www.jointcommission.org/facts_about_joint_commission_accreditation_standards
- The Joint Commission. Certification for palliative care programs. Available online: http://www.jointcommission.org/certification/palliative_care.aspx
- National Consensus Project for Quality Palliative Care. Clinical practice guidelines for quality palliative care. 3rd ed. Pittsburgh, PA; 2013. Available online: https://www.hpna.org/multimedia/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf
- Dumanovsky T, Augustin R, Rogers M, et al. The Growth of Palliative Care in U.S. Hospitals: A Status Report. J Palliat Med 2016;19:8-15. [Crossref] [PubMed]
- Granek L, Krzyzanowska MK, Tozer R, et al. Oncologists' strategies and barriers to effective communication about the end of life. J Oncol Pract 2013;9:e129-35. [Crossref] [PubMed]
- Gibbs KD Jr, Mahon MM, Truss M, et al. An Assessment of Hospital-Based Palliative Care in Maryland: Infrastructure, Barriers, and Opportunities. J Pain Symptom Manage 2015;49:1102-8. [Crossref] [PubMed]
- Zimmermann C, Wennberg R. Integrating palliative care: a postmodern perspective. Am J Hosp Palliat Care 2006;23:255-8. [Crossref] [PubMed]
- Kelley AS, Morrison RS. Palliative Care for the Seriously Ill. N Engl J Med 2015;373:747-55. [Crossref] [PubMed]
- Beck DE, Margolin DA. Physician coding and reimbursement. Ochsner J 2007;7:8-15. [PubMed]
- Ben-Chetrit E, Chen-Shuali C, Zimran E, et al. A simplified scoring tool for prediction of readmission in elderly patients hospitalized in internal medicine departments. Isr Med Assoc J 2012;14:752-6. [PubMed]
- Gilboy N, Tanabe P, Travers D, et al. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook 2012 Edition. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/esi/esihandbk.pdf
Cite this article as: Kennedy L, BrintzenhofeSzoc K. The creation of a certified palliative care program in a community hospital through education. J Hosp Manag Health Policy 2018;2:11.